JAMA:意外!近期使用NOACs与rt-PA治疗的急性缺血性中风患者的颅内出血无关!
2022-03-03 MedSci原创 MedSci原创
在接受静脉阿替普酶治疗的急性缺血性卒中患者中,与不使用抗凝剂相比,在之前的7天内使用NOACs与颅内出血的风险明显增加无关。
目前的指南建议对正在服用非维生素K拮抗剂的口服抗凝剂(NOACs)的急性缺血性卒中患者不使用静脉注射阿替普酶。
为了评价与未服用长期抗凝剂的患者相比,静脉注射阿替普酶在卒中前服用NOACs的患者中的安全性和功能结果。来自杜克大学医学中心神经病学的专家开展相关研究,结果发表在JAMA杂志上。

研究人员对163038名急性缺血性卒中患者进行回顾性队列研究,这些患者在2015年4月至2020年3月期间在1752家医院接受了静脉阿替普酶治疗,在卒中前服用NOACs或未服用抗凝剂。暴露因素为在阿替普酶治疗前7天内,用NOACs进行预中风治疗。主要结果是静脉注射阿替普酶后36小时内发生的有症状的颅内出血。有4个次要的安全结果,包括住院病人的死亡率,以及出院时评估的7个次要功能结果,包括出院回家病人的比例。
在163038名接受静脉阿替普酶治疗的患者中(中位年龄=70;49.1%为女性,2207人(1.4%)在中风前服用NOACs,160831人(98.6%)没有服用抗凝剂。服用NOACs的患者年龄较大(中位年龄,75[IQR,64-82]岁,而未服用抗凝剂的患者为70[IQR,58-81]岁),心血管合并症的发生率较高,且中风情况较严重(NIHSS=10[IQR,5-17] vs 7[IQR,4-14])。
总的来说,服用NOACs的患者未调整的症状性颅内出血率为3.7%(95%CI,2.9%-4.5%),而未服用抗凝剂的患者为3.2%(95%CI,3.1%-3.3%)。调整了基线临床因素后,各组之间的症状性颅内出血风险没有显著差异(OR=0.88[95%CI,0.70-1.10];风险差异[RD],-0.51%[95%CI,-1.36%至0.34%])。
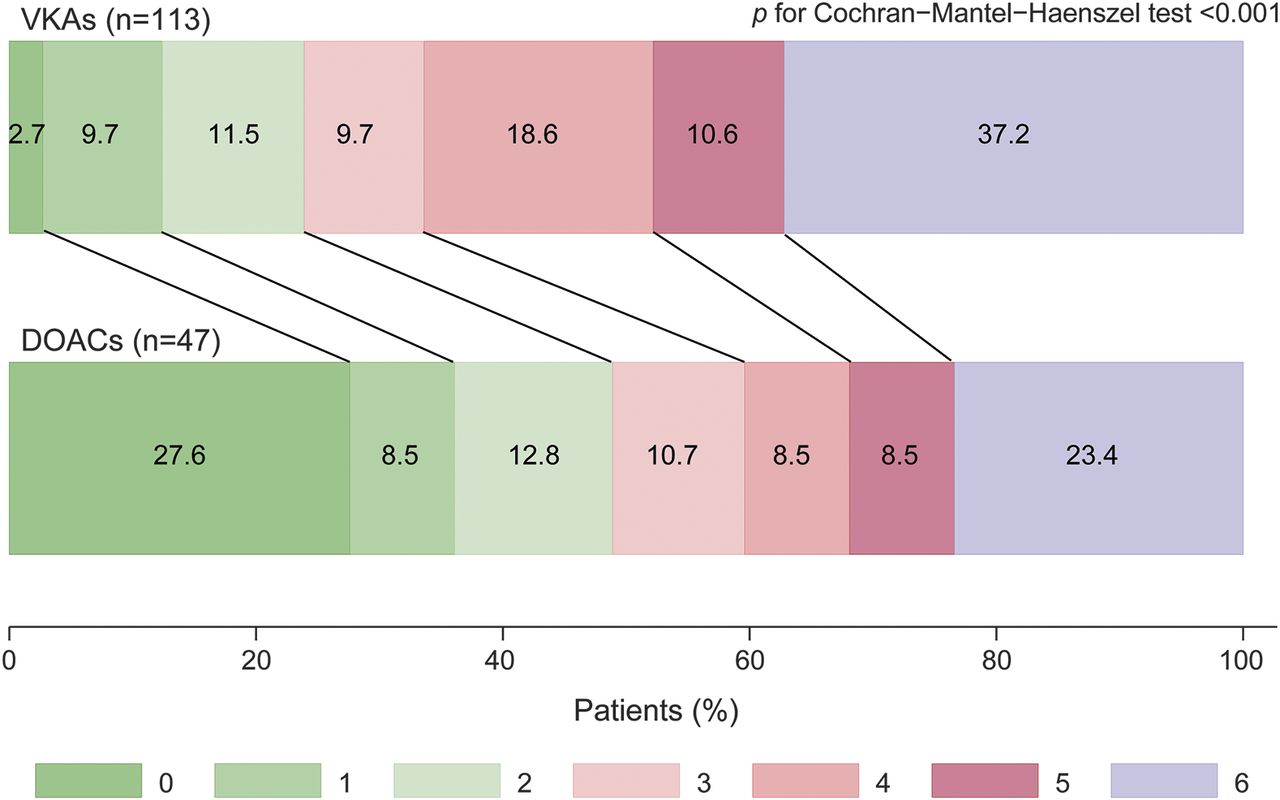
同时,次要安全结果没有明显差异,包括住院病人死亡率(服用NOACs vs 未服药6.3%vs4.9%;OR=0.84[95%CI,0.69-1.01])。在次要功能结果中,7个中的4个在调整后显示出有利于NOAC组的显著差异,包括出院回家的患者比例(45.9% vs 53.6%;OR=1.17 [95% CI,1.06-1.29];RD=3.84% [95% CI,1.46%-6.22%])。
在接受静脉阿替普酶治疗的急性缺血性卒中患者中,与不使用抗凝剂相比,在之前的7天内使用NOACs与颅内出血的风险明显增加无关。
参考文献:
Association of Recent Use of Non–Vitamin K Antagonist Oral Anticoagulants With Intracranial Hemorrhage Among Patients With Acute Ischemic Stroke Treated With Alteplase. JAMA. 2022;327(8):760–771. doi:10.1001/jama.2022.0948
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言















#急性缺血性中风#
37
#t-PA#
50
#缺血性#
34
很不错的研究发现,学习了,非常感谢
35
#rt-PA#
48
学习
51
学到了
55
#ACS#
23
#缺血性中风#
29
#NOAC#
38