Blood:转铁蛋白的N/C叶特异性调节红细胞的生成和对EPO的反应性
2019-08-26 MedSci MedSci原创
转铁蛋白,是血浆中主要的铁结合分子,与细胞表面受体相互作用,传递铁,调节铁调素的表达和红细胞生成。转铁蛋白通过两个同源叶(N和C)中的一个或两个结合与释放铁。研究人员推测N叶和C叶中铁质占用的会特异性影响转铁蛋白的功能,为验证该推论,Parrow等人建立N叶或C叶铁结合缺陷的突变小鼠(TfN-bl或TfC-bl)。
与转铁蛋白的C叶相比,N叶的铁占有具有明显的功能特性
转铁蛋白的单分子形式影响铁调素的表达和机体对促红细胞生成素的反应性
摘要:
转铁蛋白,是血浆中主要的铁结合分子,与细胞表面受体相互作用,传递铁,调节铁调素的表达和红细胞生成。转铁蛋白通过两个同源叶(N和C)中的一个或两个结合与释放铁。研究人员推测N叶和C叶中铁质占用的会特异性影响转铁蛋白的功能,为验证该推论,Parrow等人建立N叶或C叶铁结合缺陷的突变小鼠(TfN-bl或TfC-bl)。
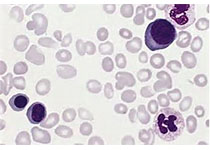
任何一种突变的纯合小鼠都有肝细胞铁负荷和肝铁调素表达降低(相对于铁浓度),虽然降低程度不同。两种小鼠模型都表现出铁限制红细胞生成的某些方面,包括原卟啉锌水平升高、血红蛋白水平下降和小红细胞增多。
此外,TfN-bl/N-bl小鼠也表现出了预期的铁限制对红细胞生成的影响作用(如促红细胞生成素升高,但RBC计数无增加),同时对外源性促红细胞生成素的反应差。与此相反,TfC-bl/C-bl小鼠表现为RBC计数升高,对外源性促红细胞生成素的反应过度,且足以改善贫血。
最后,杂合小鼠的表现进一步支持相对的N叶和C叶铁占用在转铁蛋白介导的铁稳态和红细胞生成调控中的作用。
原始出处:
Nermi L. Parrow, et al.Lobe specificity of iron-binding to transferrin modulates murine erythropoiesis and iron homeostasis.Blood 2019 :blood.2018893099; doi: https://doi.org/10.1182/blood.2018893099
本文系梅斯医学(MedSci)原创编译,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#特异性#
26
#反应性#
37
#红细胞#
31
#转铁蛋白#
39
学习了
82
谢谢了,学习
85
好
71