European Radiology:人工耳蜗植入术后乳突面神经管的影像学评估与面神经刺激的相关性
2022-01-20 shaosai MedSci原创
人工耳蜗(CI)手术是现阶段治疗严重感音神经性听力障碍的主要治疗手段。

人工耳蜗(CI)手术是现阶段治疗严重感音神经性听力障碍的主要治疗手段。然而,由于面部凹陷位于CI的插入平面内,因此面部神经可能会受到设备的刺激,表现为受影响一侧的异常感觉或眨眼,该电刺激被称为面部神经刺激(FNS),发生率在0.9-14.9%之间。
许多研究者对术后FNS的发生有不同的解释。先前的研究表明,电流可能会绕过耳蜗的基底转弯,刺激附近的面神经迷宫段,特别是在骨质阻抗降低的情况下更为显著。还有人认为FNS与年龄小、耳蜗异常、CI设备类型以及长期听觉剥夺患者所需的高刺激电流有关。由于电极电缆和某些情况下耳蜗外电极的存在可能与乳突面神经管有直接关系,所以乳突面神经可能与FNS病例有关;然而,迄今为止,尚未有研究对FNS病例的乳突面神经进行影像学评估。
近日,发表在European Radiology杂志的一项研究探讨了面部凹陷区乳突面神经管的术后影像学评估及其与人工耳蜗的关系以及其他可能导致FNS的临床或植入物相关风险因素与CI手术后患者的FNS发生情况之间的关系,为减少FNS的发生率提供了影像学参考依据。
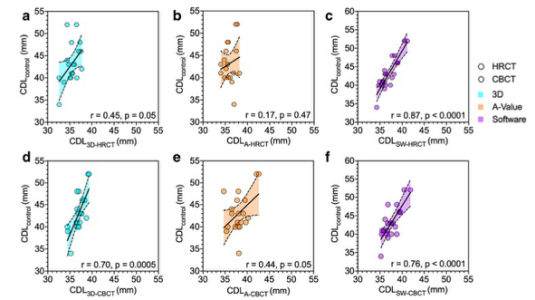
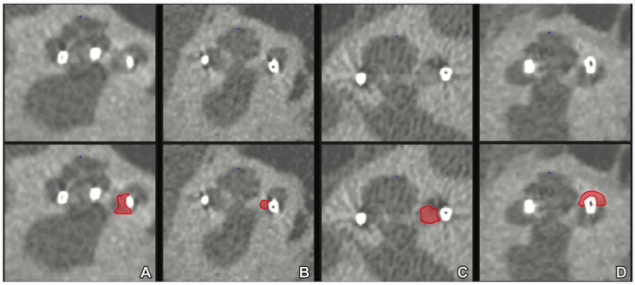
由两位经验丰富的放射科医生回顾性地评估了215次术后CI CBCT检查。评估了乳突面管直径、壁厚、电极电缆与乳突面管之间的距离以及面鼓角。此外,还评估了耳蜗内的位置以及电极的插入角度和深度。临床数据分析了术后1.5年内的FNS、CI类型、发病情况和听力损失的原因,如耳硬化症、脑膜炎和以前的耳部手术史。使用逻辑回归法将术后FNS与测量和临床数据相关联。
在研究人群中(平均年龄:56±18岁),有10名患者出现了FNS。FNS与面管直径(p = 0.09)、管壁厚度(p = 0.27)、与CI线的距离(p = 0.44)以及与鼓索的角度(p = 0.75)之间的相关性在统计学上并不显著。脑膜炎/脑炎史(p = 0.001)、耳蜗外电极接触(p = 0.002)、耳蜗位置(p = 0.02)、年轻患者的年龄(p = 0.03)、侧壁电极类型(p = 0.04)和早期/儿童发病的听力损失(p = 0.04)都有统计意义。脑膜炎/脑炎和耳蜗外电极接触的病史被纳入多变量逻辑回归的前两步。
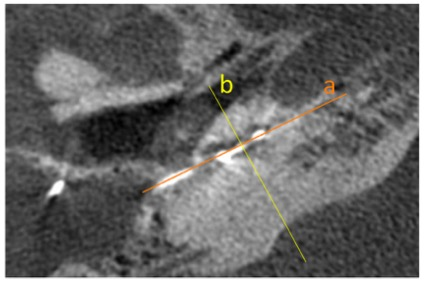
图 轴向CBCT图像显示了不同的重建平面。(a)平行于耳蜗基底转的耳蜗视图重构,(b)垂直于耳蜗视图平面的中二极视图重构。
本研究数据表明,乳突面神经管的影像学评估及其与面凹处CI电极的位置关系不是术后FNS发生的预测因素。然而,影像学上可检测到的耳蜗外电极接触和脑膜炎/脑炎病史为最重要的两个预测因素。偏离耳蜗内理想电极位置的鼓室、侧壁-CI型、年轻患者的年龄和SNHL的早期发病也可作为术后FNS的重要风险因素。
原文出处:
Iris Burck,Rania A Helal,Nagy N N Naguib,et al.Postoperative radiological assessment of the mastoid facial canal in cochlear implant patients in correlation with facial nerve stimulation.DOI:10.1007/s00330-021-08128-w
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#PE#
43
#相关性#
82
#面神经#
42
#人工耳蜗#
50
#神经刺激#
46
#植入#
36
#耳蜗植入#
32
#影像学评估#
51