J Dent Res:牙科手术后菌血症的预防:一项互联网meta分析
2019-09-08 lishiting MedSci原创
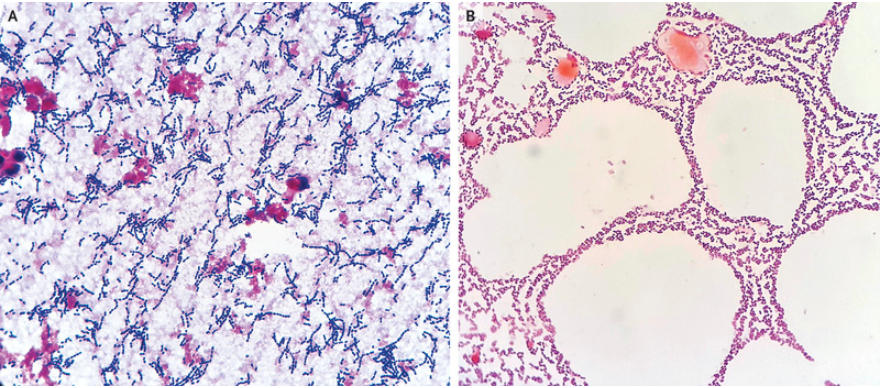
牙科手术后菌血症经常发生并且十分令人烦恼。而多种预防措施之间的效果比较还未可知。这篇研究的目的是为了比较牙科手术后菌血症的多种干预措施的预防效果。
牙科手术后菌血症经常发生并且十分令人烦恼。而多种预防措施之间的效果比较还未可知。这篇研究的目的是为了比较牙科手术后菌血症的多种干预措施的预防效果。研究对ClinicalKey, Cochrane CENTRAL, Embase, ProQuest, PubMed, ScienceDirect, Web of Science和ClinicalTrials.gov数据库自2018年12月4日起的文献进行检索和回顾。选择评估预防牙科术后菌血症干预措施的随机对照试验。研究共纳入了包含2,147受试者的24项试验。作者的互联网meta分析结果显示,与安慰剂/对照组相比,在所有干预措施中静脉注射1,000/200 mg的阿莫西林/克拉维酸发生牙科术后菌血症的几率最低(odds ratio = 0.03, 95% CI = 0.00 to 0.63)。与安慰剂/对照组相比,在所有口服或局部用药的干预措施中口服3 g阿莫西林发生牙科术后菌血症的几率最低(odds ratio = 0.10, 95% CI = 0.02 to 0.44)。没有发生严重副作用的报道,比如:过敏性休克、死亡和耐药菌的产生。所
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#Meta#
25
#MET#
22
好
59
#互联网#
31
#菌血症#
39
#牙科#
32
学习了很有用不錯
68
好
65
学习了,谢谢分享
56