Clinical Nutrition: 补充姜黄素对血液透析患者炎性转录因子表达的影响
2020-12-05 MedSci原创 MedSci原创
慢性肾脏病(CKD)患者会出现很多常见临床并发症和合并症,例如糖尿病,高血压,全身性疾病,免疫疾病,持续尿毒症和营养不良,这些与氧化应激和炎症增加有关。
慢性肾脏病(CKD)患者会出现很多常见临床并发症和合并症,例如糖尿病,高血压,全身性疾病,免疫疾病,持续尿毒症和营养不良,这些与氧化应激和炎症增加有关。炎症和氧化应激是尿毒症表型的常见特征,其特征在于活性氧(ROS)的产生与抗氧化能力之间的不平衡。随着ROS产量的增加,转录因子kB(NF-kB)被激活,这与炎症反应的刺激以及诸如肿瘤坏死因子(TNF)和白介素(IL)等细胞因子的释放有关。

炎症反应的另一个重要调节剂,含有Nod样受体的3(NLRP3),是NLR(核苷酸结合结构域和富含亮氨酸的结构域,含有重复序列)家族的成员,最近在CKD中得到了大量研究。炎性小体NLRP3介导caspase-1,IL-18和IL-1β的裂解和激活,进而导致复杂的细胞反应网络引发局部和全身性炎症反应,具体来说,当线粒体膜破裂时,各种线粒体成分(例如导致氧化应激的DNA和蛋白质)被释放,从而激活NF-kB和NLRP3寡聚,产生炎症。
CKD患者的核转录因子-类红细胞因子2(Nrf2)表达下调,导致抗氧化反应降低,导致抗氧化酶生成降低,并在氧化应激和促炎 过度生成之间形成恶性循环细胞因子,最近有报道,CKD5中Nrf2的表达降低与线粒体衍生肽的肌肉表达降低有关。姜黄素是从姜黄根(姜黄科)的根中提取的天然酚类化合物,由于其作为抗炎和天然抗氧化剂的潜在应用而被广泛研究。因此,本项研究的目的是评估姜黄素汁对血液透析(HD)患者炎症转录因子表达的影响。
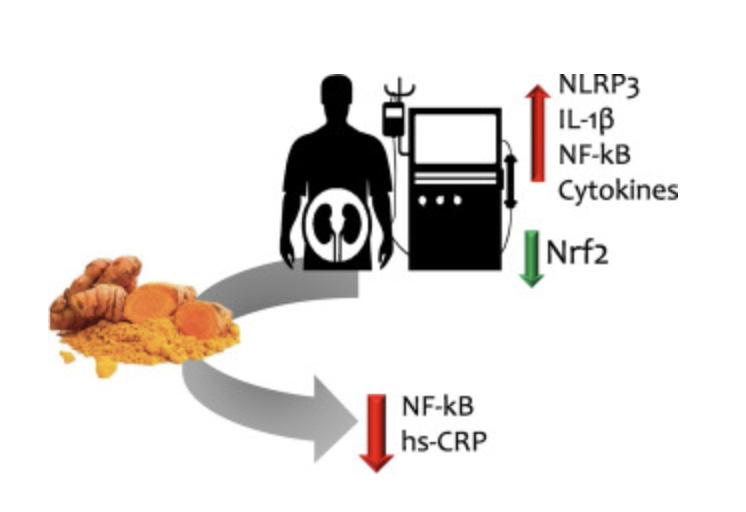
本项研究共纳入31位HD患者,分为两组:姜黄素组(每个透析疗程/每周接受3个月后分别接受100 mL橙汁,12 g胡萝卜和2.5 g姜黄)和对照组(接受不含姜黄素的相同果汁治疗);每组都有14位患者完成了研究。研究人员对所有患者的Nrf2,NF-kB,NLRP3炎性小体和IL-1β在外周血单个核细胞和常规生物化学,食物摄入量均进行了测量比较。补充三个月后,姜黄素组显示NF-kB mRNA表达显着降低[从1.08(0.77–1.38)降至0.52(0.32–0.95),p = 0.02],血浆高敏C反应性蛋白质(hsCRP)的水平[从3.8(2.5–6.8)降到2.0(1.1–3.8)mg / L,p = 0.04]。其他评估指标没有变化。
由此,研究人员证实接受HD治疗的CKD患者接受姜黄素治疗三个月后,炎症标志物,NF-kB mRNA表达和hsCRP降低,这表明口服姜黄素可能对该患者组具有抗炎作用。
原始出处:
Livia Alvarenga. Et al. Impact of curcumin supplementation on expression of inflammatory transcription factors in hemodialysis patients: A pilot randomized, double-blind, controlled study. Clinical Nutrition.2020.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#nutrition#
28
#转录#
34
#血液透析#
0
#clinical#
35
#转录因子#
35
#透析患者#
32
学习
77