Nature:又一力证,炎症驱动阿尔茨海默症
2019-11-27 佚名 中国生物技术网
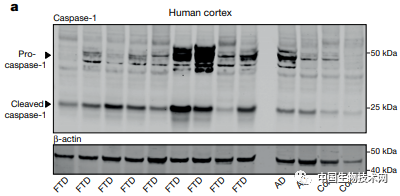
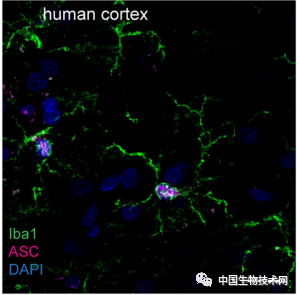
近日,发表在《Nature》上的一篇研究中,来自德国神经退行性疾病中心(DZNE)和波恩大学领导的国际研究团队发现了一种炎症机制,似乎在阿尔茨海默症(AD)和其他脑部疾病的毒性tau蛋白形成过程中发挥了关键作用。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#阿尔茨#
27
#Nat#
35
#阿尔茨海#
36
#阿尔茨海默#
33
研究很前沿,受益良多
97
好
85
好好好好好好
84