Translational Psychiatry:血清素或可成为抑郁症疗效新标准
2021-05-11 梅斯医学 MedSci原创
血清素系统的变化是抑郁症生物学的一部分,而且这种变化与抑郁症发作有关,也就是说,血清素系统的变化不是一种静态特征,当抑郁症情况有所缓解,血清素升高。
血清素(Serotonin,简称为5-HT)为单胺型神经递质,由色氨酸经色氨酸羟化酶转化为5-羟色氨酸,再经5-羟色氨酸脱羧酶在中枢神经元及动物(包含人类)消化道之肠嗜铬细胞中合成。
Pixabay
血清素主要存在于动物(包括人类)的胃肠道、血小板和中枢神经系统中,在大脑中的含量为总量的2%。医学界普遍认为血清素与幸福和快乐感觉有关。大脑中血清素的低水平被视为抑郁症的一个可能原因,许多抗抑郁药通过阻断一种将血清素从神经细胞中转运出去的蛋白质而发挥作用。
许多现代抗抑郁药物抑制这种转运器,从而增加突触中血清素的浓度。然而,这些药物的效果可能会延迟几周,在某些情况下,它们根本没有效果,因此迫切需要新的或改进的药物治疗方法。为了实现这一目标,需要对该疾病的生物学原因有更多的了解。
近日,卡罗林斯卡学院的一项大脑成像研究现在显示,在一组经过认知行为治疗后从抑郁症中恢复的17人中,血清素转运体的平均水平有所提高。该结果发表在《转化精神病学》杂志上。

在这项研究中,研究人员试图调查当抑郁症患者被成功治疗时,血清素转运体如何变化。为此,研究者测量了17名抑郁症患者在接受基于互联网的认知行为疗法前后的血清素水平,并招募17名无抑郁症参与者作为对照组进行比较。在治疗之前,抑郁症患者的血清素平均水平与17名健康人组成的对照组大致相同。
测量是通过正电子发射断层扫描(PET)这种大脑成像技术实现,科学家可以通过放射性示踪剂测量大脑中不同物质的水平。
研究发现,经过三个月的治疗,抑郁症患者的血清素的水平平均提高了10%,17名患者中有13人报告说他们的症状有了明显的改善。
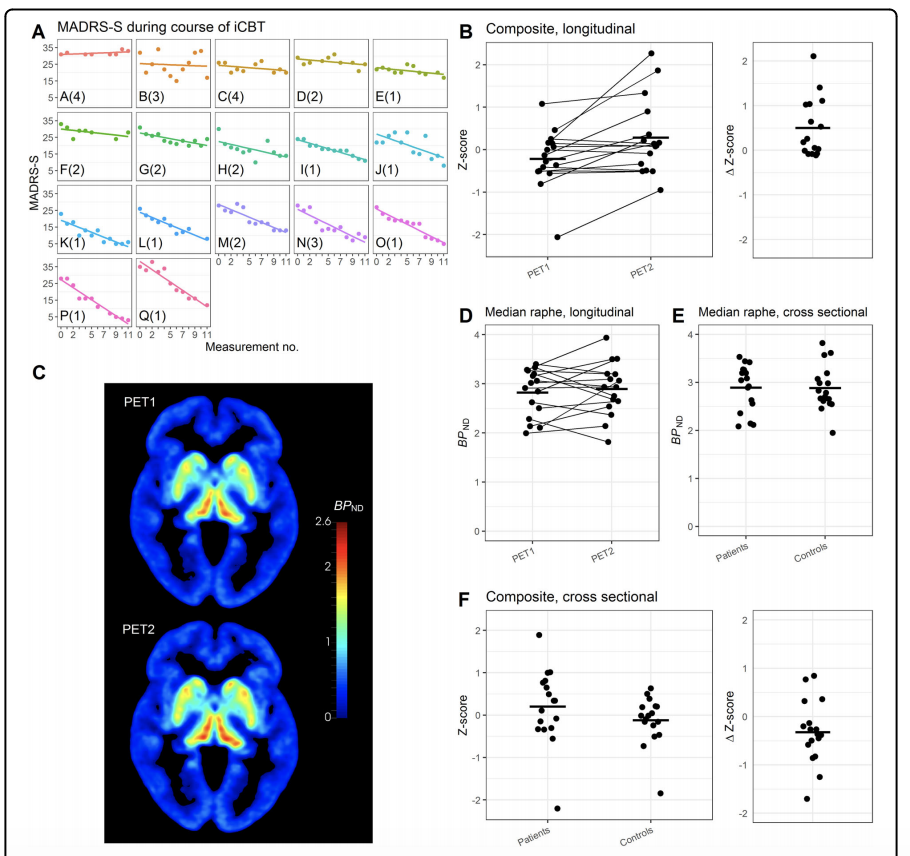
PET数据
研究结果表明,血清素系统的变化是抑郁症生物学的一部分,而且这种变化与抑郁症发作有关,也就是说,血清素系统的变化不是一种静态特征,当抑郁症情况有所缓解,血清素升高。
该研究的通讯作者、卡罗林斯卡学院临床神经科学系的研究员约翰-伦德伯格表示,这一发现提出了许多关于血清素系统在抑郁症中的功能的问题,并为可能挑战血清素和抑郁症的普遍概念的研究思路开辟了道路。
该研究的第一作者Jonas Svensson针对该研究指出,从现在研究结果来看,血清素系统并不导致抑郁症,而是大脑保护自己免受抑郁症影响的防御机制的一部分。就像当一个人受到压力时,例如在抑郁状态下,血清素水平下降,而当这种压力消失时,血清素水平会上升或正常化。
然而,需要提出的是,该研究存在一定的局限性,比如研究样本较少。目前,研究人员现在正在设计新的研究,以测试血清素系统的动态功能是否能成为压力防御系统的一部分。
原始出处:
"Serotonin transporter availability increases in patients recovering from a depressive episode," Jonas E. Svensson, Cecilia Svanborg, Pontus Plavén-Sigray, Viktor Kaldo, Christer Halldin, Martin Schain and Johan Lundberg, Translational Psychiatry, online May 10, 2021, DOI: 10.1038/s41398-021-01376-w
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言















#translational#
41
#新标准#
50
#TRA#
42
值得学习
57
#Psychiatry#
41
#Transl#
36
#Translation#
31
谢谢梅斯提供这么好的信息,学到很多
51
不错好文
63