肺癌时最常见的癌症死亡原因,估计全球每年的发病率为180万,死亡率为160万。研究表明,没有致癌驱动基因突变的非小细胞肺癌(NSCLC)蕴藏着大量的体细胞突变,这些突变是宿主免疫的抗原性目标。
逃避免疫破坏是肺癌发展的一个关键机制,并被Hanahan和Weinberg在2011年描述为癌症的一个新标志。肿瘤细胞和宿主免疫之间的关系通常有利于肿瘤的消除或免疫破坏和肿瘤生长之间的平衡,但当肿瘤细胞发展到免疫逃逸时,这些癌细胞会克服宿主免疫,用免疫抑制环境保护自己,并发生转移,造成致命的后果。
T细胞上的程序性细胞死亡受体1(PD-1)和肿瘤细胞上的程序性细胞死亡配体1(PD-L1)之间的相互作用在免疫逃逸中起着重要作用。PD-1和PD-L1抑制剂,被称为PD-1阻断,已经被确立为晚期NSCLC患者治疗的标准疗法。
一些患者经历了持久的肿瘤反应,但其他患者没有获得临床益处,这突出了识别生物标志物以改善患者选择的重要性。PD-L1在肿瘤细胞上的表达与否,仍然是报道最多的与PD-1阻断的抗肿瘤活性有关。
近日,来自澳大利亚悉尼癌症转化研究中心的专家对MEDLINE、EMBASE的论文进行系统检索,以了解抗PD-1或抗PD-L1单药治疗转移性NSCLC的有效性,主要WiePD-L1亚组的客观反应率(ORR)、1年和2年无进展生存期(PFS)以及2年和3年总生存期(OS)的数据。
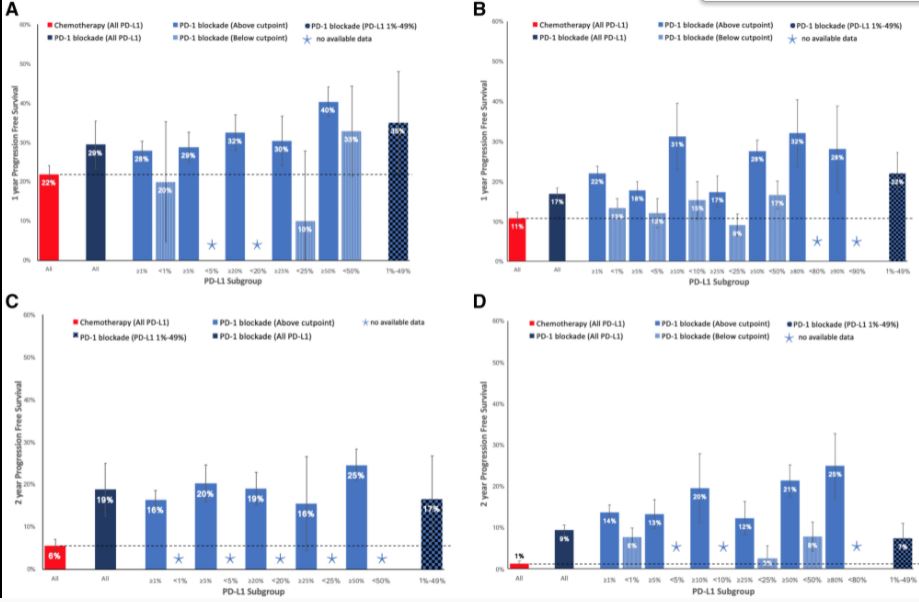
最终共有27项研究的9810名患者被纳入。在治疗无效的患者中,PD-1阻断比化疗的好处体现在PD-L1≥50%的患者的ORR,PD-L1≥1%的患者的2年OS,以及未经选择的患者的1年PFS、2年PFS和3年OS上。
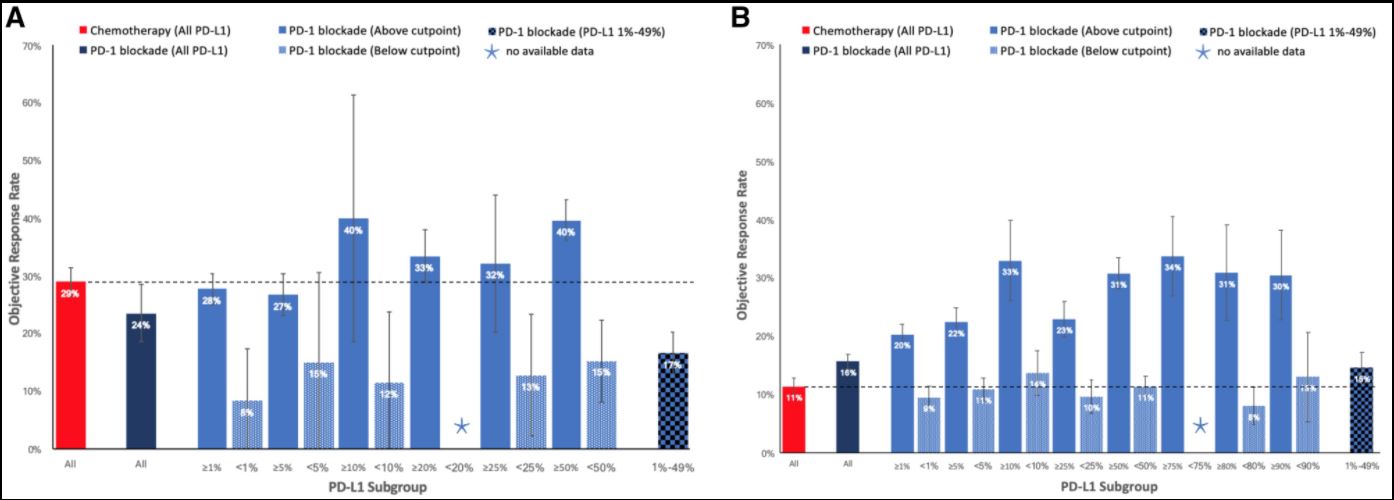
化疗或PD-1阻断在不同PD-L1亚组的ORR。A)治疗无效患者的ORR。B)以前治疗过的患者的ORR。
进一步分析显示,一线PD-1阻断治疗与化疗相比,如果PD-L1≥50%,则显示出更高的ORR、2年PFS和3年OS;如果PD-L1为1%-49%,则显示出更低的ORR、更高的2年PFS和相似的3年OS;如果PD-L1<1%,则显示出更低的ORR、相似的1年PFS和更低的2年OS。
不同PD-L1亚组中,化疗或PD-1阻断的1年和2年PFS率。A)治疗无效患者的一年PFS。B) 以前接受过治疗的患者一年的PFS。C) 未接受治疗的患者两年的PFS。D) 以前接受过治疗的患者两年的PFS。
此外,在以前治疗过的患者中,PD-1阻断疗法在所有PD-L1亚组中表现出与化疗相似或更优的结果。
综上,PD-L1无效患者应根据自身情况选择PD-1阻断疗法与化疗。在以前接受过治疗的患者中,PD-1阻断疗法在所有PD-L1亚组中提供了比化疗有利的结果。
参考文献:
Response Rate and Survival at Key Timepoints With PD-1 Blockade vs Chemotherapy in PD-L1 Subgroups: Meta-Analysis of Metastatic NSCLC Trials. https://doi.org/10.1093/jncics/pkab012.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#SCLC患者#
22
#转移性NSCLC#
29
#NCI#
39
#转移性#
27
#NSCLC患者#
28
NSCLC下一步突破在于新靶点了,靶向治疗和免疫治疗基本见顶了,再有新的就需要新机制了
50
不错哈哈哈哈
62