Neurology:取栓后24h血压目标值,5000例患者的数据分析
2022-02-15 杨中华 “ 脑血管病及重症文献导读”公众号
在最近一项观察性队列研究的配对荟萃分析中,患者的预后与EVT术后血压水平的关系比术前或围手术期血压更密切。同样,在各自的时间间隔内,收缩压的相关性比舒张压的相关性更强。
尽管血管内血栓切除术(endovascular thrombectomy,EVT)是迄今为止唯一可用于改善由颅内大血管闭塞(large vessel occlusion,LVO)引起的急性缺血性卒中(acute ischemic stroke,AIS)发病率和死亡率的手术治疗方法,在血管内手术结束后成功再灌注的患者中,约有一半死亡或永久残疾。
在接受急性再灌注治疗的患者中,EVT后的血压(BP)管理可能是改善神经功能预后的一个变量。对于接受EVT的LVO患者,指导BP管理的数据有限,对于EVT手术之前、期间和之后的最佳BP目标,也没有明确的共识。尽管目前的指南建议在EVT期间和EVT后的前24小时内,收缩压目标为<=180毫米汞柱,舒张压105毫米汞柱,他们还强调了缺乏证实这一立场的随机试验。这些血压目标值来自于静脉溶栓的临床试验,静脉溶栓的成功再灌注的可能性较小,而EVT时可以实时确认动脉是否再通,所以这些血压目标值可能不适合EVT。此外,在真实世界中,不同中心对EVT后的BP目标值存在很大差异。
在最近一项观察性队列研究的配对荟萃分析中,患者的预后与EVT术后血压水平的关系比术前或围手术期血压更密切。同样,在各自的时间间隔内,收缩压的相关性比舒张压的相关性更强。
2022年1月来自加拿大的Aristeidis H. Katsanos等在Neurology上公布了他们的研究结果,该研究对已发表的观察性研究进行了个体患者数据的荟萃分析(Individual Patient Data Meta-analysis,IPD-MA),进一步评估了前循环LVO的AIS患者EVT后血压水平与临床结局之间的相关性。
方法:主要纳入标准包括,年龄大于18岁的AIS患者,接受了成功或失败的EVT治疗,并且提供了EVT手术结束后的个体或平均24小时收缩压值。
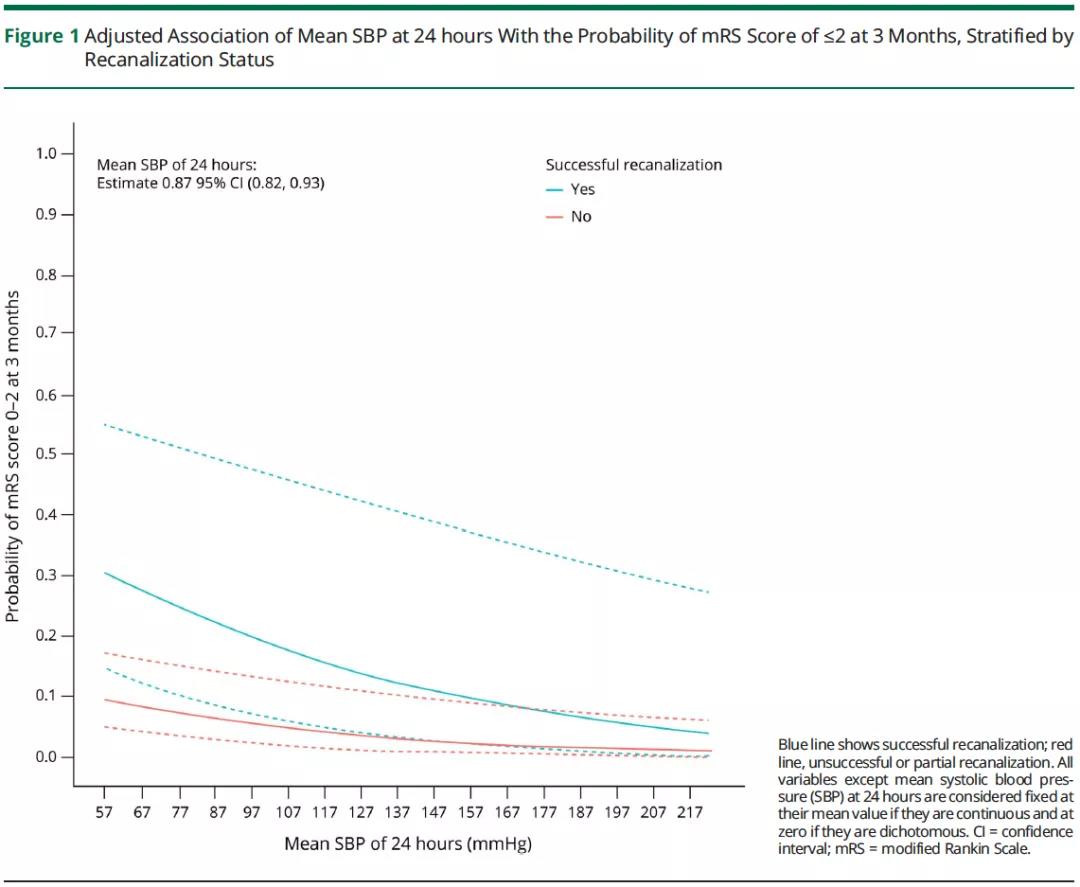
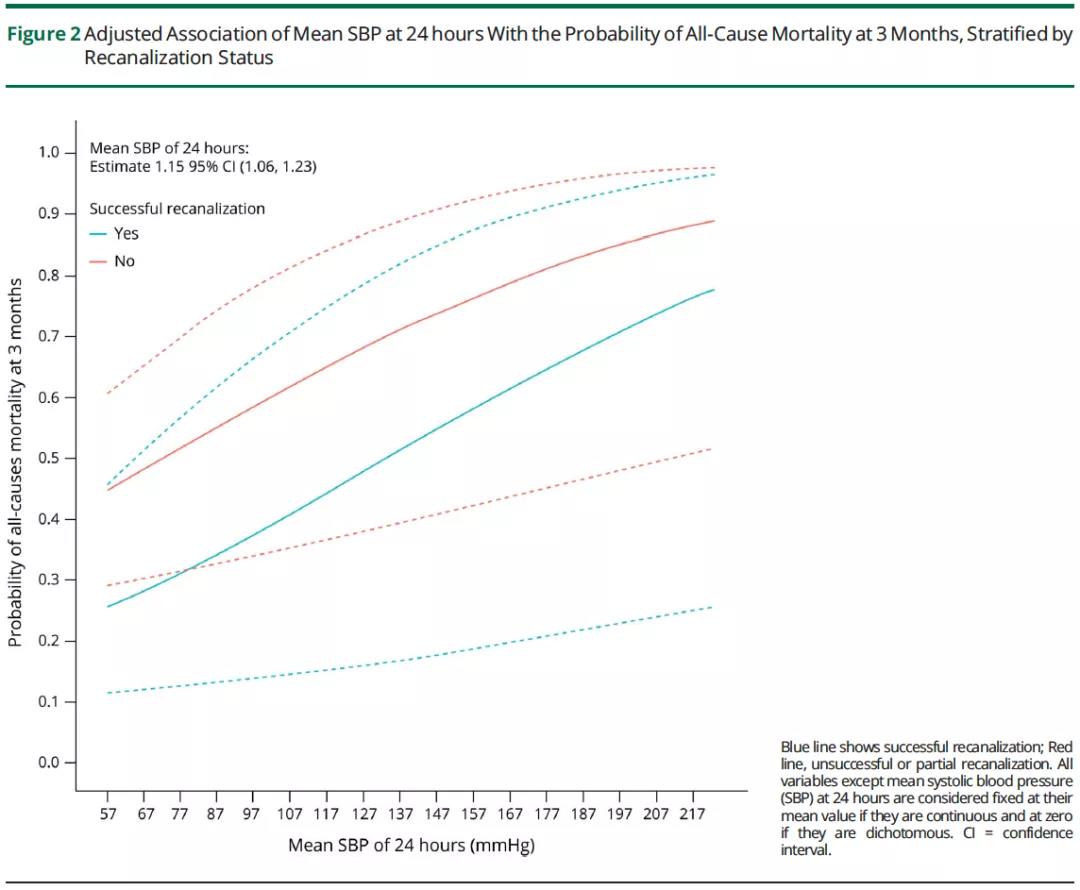
共纳入7项研究的5874名患者(平均年龄69岁+-14;50%为女性;入院时NIHSS中位数16分)。在EVT结束后的前24小时内,平均收缩压水平每增加10毫米汞柱与较低几率的功能改善有关(未经调整的共同优势比[OR]0.82,95%可信区间[CI]0.80–0.85;调整共同优势比0.88,95%可信区间0.84–0.93),和较低比例的mRS≤2有关(未调整OR 0.82,95%可信区间0.79-0.85;调整OR 0.87,95%可信区间0.82-0.93),以及和较高比例的3个月时全因死亡率有关(未调整OR 1.18,95%可信区间1.13-1.24;调整OR 1.15,95%可信区间1.06-1.23)。
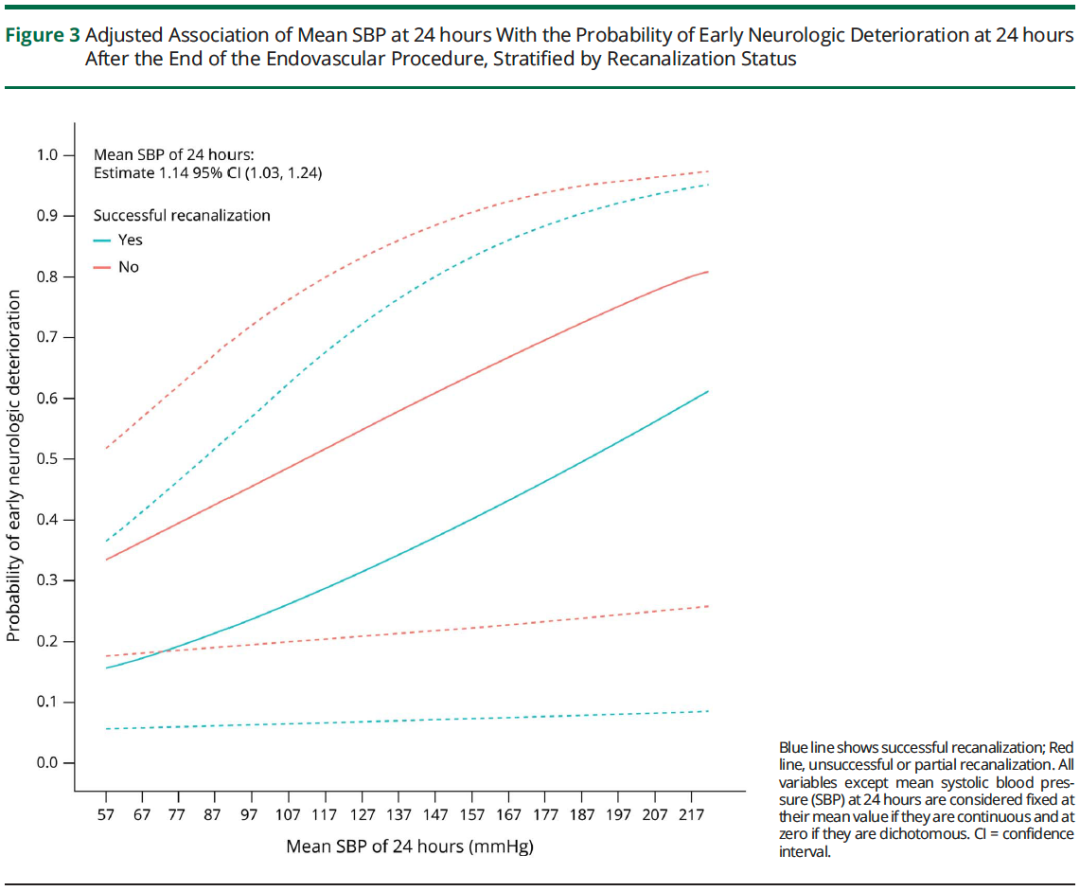
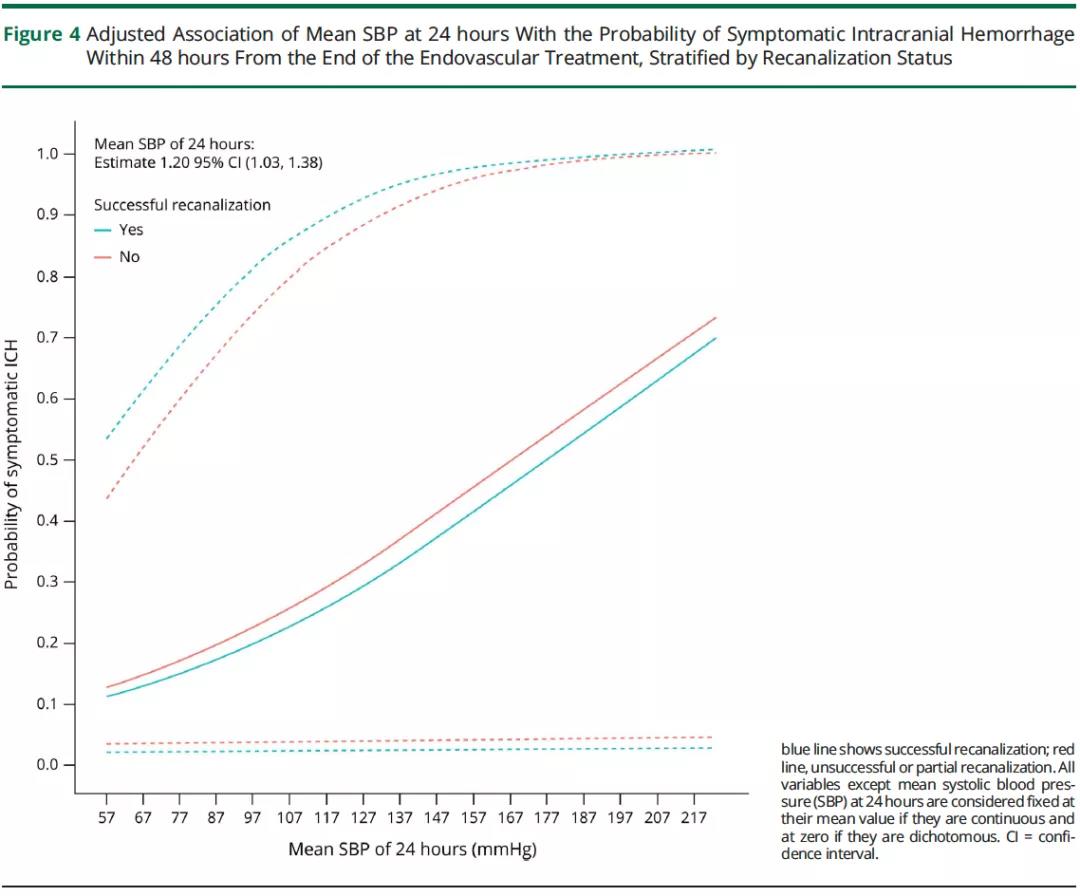
较高水平的24小时平均收缩压也与EVT后早期神经功能恶化(未经调整的OR 1.14,95%可信区间1.07-1.21;经调整的OR 1.14,95%可信区间1.03-1.24),以及症状性颅内出血(未经调整的OR 1.20,95%可信区间1.09-1.29;经调整的OR 1.20,95%可信区间1.03-1.38)的可能性增加有关。EVT的再通状态对上述关系没有影响。
最终作者认为,EVT术后前24小时内平均收缩压水平升高与症状性颅内出血、早期神经功能恶化、3个月死亡率和3个月功能转归恶化的几率增加独立相关。
译者注:取栓第一个24h内的血压管理存在很大争论,不同研究得到了不同甚至是相反的结果,还需要设计精良的随机对照研究回答这个问题。
原始出处:
Aristeidis H. Katsanos, Konark Malhotra, Niaz Ahmed, et al. Blood Pressure After Endovascular Thrombectomy and Outcomes in Patients With Acute Ischemic Stroke: An Individual Patient Data Meta-analysis. Neurology. 2022 Jan 18;98(3):e291-e301. doi: 10.1212/WNL.0000000000013049. Epub 2021 Nov 12.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#血压目标值#
37
#取栓#
39
赞
58
#Neurol#
42