Cell:CAR-T被改造后有望攻克艾滋病
2019-12-02 BioWorld BioWorld
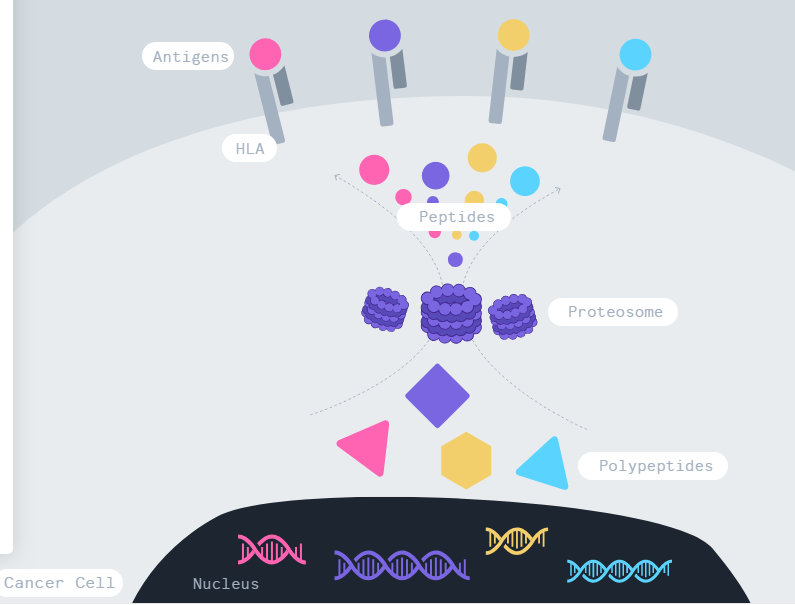
CAR-T,全称是Chimeric Antigen Receptor T-Cell Immunotherapy,指的是嵌合抗原受体T细胞免疫疗法。简单一点说,CAR-T就是把病人的免疫T细胞在体外通过生物技术改造,令其识别肿瘤细胞表面的抗原,然后把这些细胞输回病人体内,达到识别、杀死癌细胞的治疗效果。2017年,美国食品药品监督管理局FDA先后批准了两款CAR-T细胞疗法上市,用于治疗白血病和
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#CEL#
19
#Cell#
30
#CAR-#
33
学习了,谢谢分享
70
学习了,谢谢分享
58
学习了,谢谢分享
59
学习了,谢谢分享
60