Otolaryngol Head Neck Surg:怀孕、雌激素暴露和耳硬化症的发展:1196名妇女的病例对照研究
2020-11-04 Ale'x'Y'ang MedSci原创
最近,有研究人员确定了妊娠史或双侧眼球切除术是否与随后的耳硬化症发展或疾病严重程度有关。
最近,有研究人员确定了妊娠史或双侧眼球切除术是否与随后的耳硬化症发展或疾病严重程度有关。
研究是一个基于人群的病例对照研究,共包括了1196名妇女:299例耳硬化症和897名匹配的对照。研究发现,≥1次分娩与耳硬化症关联的让步比为1.16(95%CI 0.85-1.60;P=0.35)。1次、2次、3次或≥4次分娩与耳硬化症关联的让步比分别为1.22(0.83-1.80)、1.09(0.71-1.68)、1.28(0.77-2.12)和1.00(0.54-1.84)。先前双侧眼球切除术与耳硬化症相关的让步比为1.12(0.58-2.18;P=0.73)。在有耳硬化症的病例中,与没有耳硬化症的病例相比,有≥1次分娩的女性在诊断时的PTA并未显著更高(中位数45dB听力损失[HL][四分位数范围{IQR}36-55] vs 43 [IQR 34-53];P=0.18);但有双侧眼球切除术的女性在诊断时的PTA与没有耳硬化症的女性相比显著更高(中位数54 dB HL[IQR 44-61] vs 44 [IQR 34-53];P=0.03)。
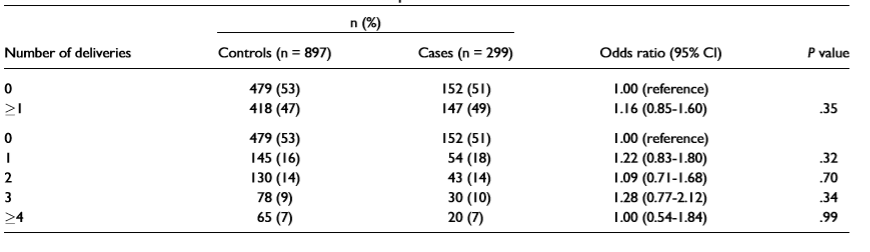
分娩次数与耳硬化症之间的相关性
最后,研究人员指出,这些数据不支持内源性雌激素暴露与耳硬化症的发展之间的关系。有怀孕史的耳硬化症妇女在诊断时听力并没有明显变差,表明怀孕与疾病严重程度没有关系。
原始出处:
Robert J Macielak , John P Marinelli , Douglas J Totten et al. Pregnancy, Estrogen Exposure, and the Development of Otosclerosis: A Case-Control Study of 1196 Women. Otolaryngol Head Neck Surg. Oct 2020
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#对照#
28
#NEC#
37
#耳硬化症#
39
#耳硬化#
37
#硬化症#
22
#病例对照#
58
#病例对照研究#
35
学习
85
了解
88