Eur Heart J:心血管疾病和全因死亡率的体力活动悖论
2021-04-09 MedSci原创 MedSci原创
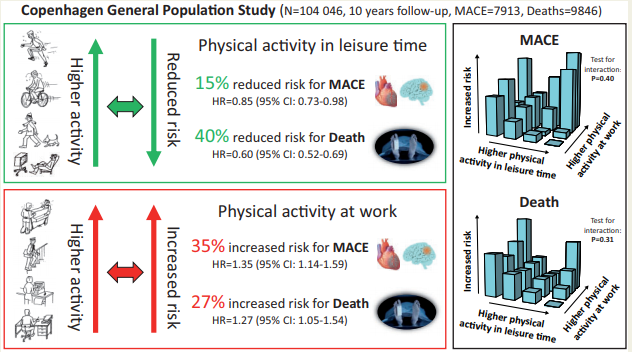
业余时间较高的体力活动与降低MACE和全因死亡风险相关,而较高的职业体力活动与其风险增加相关,两者相互独立。
业余时间体力活动与降低心血管疾病和全因死亡风险相关,但这些与职业体力活动的关系尚未明确。
近日,心血管领域权威杂志Eur Heart J上发表了一篇研究文章,研究人员旨在评估一个假设,即业余时间体力活动与减少主要不良心血管事件(MACE)和全因死亡风险相关,而职业体力活动与其增加的风险相关。
研究人员在哥本哈根一般人群研究中分析了104046名年龄在20-100岁的女性和男性,在2003-2014年期间进行了基线测量,随访的中位时间为10年。业余和职业体力活动都是基于自我报告分为四种类别。

研究人员观察到了7913人(7.6%)死于MACE,9846人(9.5%)死于各种原因。与业余时间体力活动较少相比,经多变量调整(生活方式、健康、生活条件和社会经济因素)MACE的风险比:中等强度为0.86(0.78-0.96)、高强度为0.77(0.69-0.86)和非常剧烈活动为0.85 (0.73-0.98);较高职业体力活动对应值分别为1.04(0.95-1.14)、1.15(1.04-1.28)、1.35(1.14-1.59)。在全因死亡率方面,业余时间较高的体力活动对应的风险比分别为0.74(0.68-0.81)、0.59(0.54-0.64)和0.60(0.52-0.69),职业强度较高的体力活动对应的风险比分别为1.06(0.96-1.16)、1.13(1.01-1.27)和1.27(1.05-1.54)。在不同阶层中,在生活方式、健康、生活条件和社会经济因素方面也得到了类似的结果,如果不包括随访前5年死亡的患者。体力活动的两个方面的水平对MACE的风险(P=0.40)或全因死亡率(P=0.31)没有相互作用。
由此可见,业余时间较高的体力活动与降低MACE和全因死亡风险相关,而较高的职业体力活动与其风险增加相关,两者相互独立。
原始出处:
Andreas Holtermann.et al.The physical activity paradox in cardiovascular disease and all-cause mortality: the contemporary Copenhagen General Population Study with 104 046 adults.European Heart Journal.2021.https://doi.org/10.1093/eurheartj/ehab087
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#全因死亡率#
31
#ART#
25
#血管疾病#
36
#HEART#
33
可以的!
57
学习了,很有收获
69