AJRCCM:晚期肺动脉高压阻塞性肺功能的演变
2021-09-24 刘少飞 MedSci原创
肺动脉高压 (PAH) 的特征是肺动脉阻抗增加,导致运动不耐受和右心衰竭。 随着针对右心衰竭的治疗方法的改进,人们对 PAH 降低运动能力的新途径越来越感兴趣,这是一个关键的治疗目标。
众所周知,肺动脉高压 (PAH) 的特征是肺动脉阻抗增加,导致运动不耐受和右心衰竭。 随着针对右心衰竭的治疗方法的改进,人们对 PAH治疗的新途径越来越感兴趣。虽然在PAH患者中限制性肺病的病人能被很好地识别,在先前的横断面 PAH 研究中也描述了外周气道阻塞和动态过度充气。 该研究试图描述晚期 PAH 阻塞性生理学的演变,并结合成像和组织病理学研究潜在机制。
该研究由美国学者发现发表于AJRCCM,其:
研究题目:Evolution of Obstructive Lung Function in Advanced Pulmonary Arterial Hypertension
期刊年卷:Am J Respir Crit Care Med 2021 Sep 23;
通讯作者:Rajan Saggar, MD
Division of Pulmonary and Critical Care Medicine
David Geffen School of Medicine at UCLA
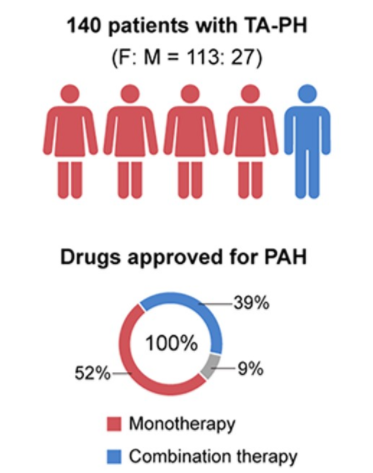
该研究PAH队列的人口统计学、肺功能、胸部影像学参数和血流动力学数据(在诊断和移植时)如表 1 所示。 患者通常为年轻、从 1993 年至 2014 年被诊断为 PAH 的不吸烟女性,并于 2004-2020年接受移植。 最终 PAH 诊断基于临床/放射学/病理学相关性,包括特发性 PAH (n=10)、肺毛细血管瘤病 (PCH) (n=2)、苯丙胺/厌食症 (n=2) 和纠正先天性 (n= 1)。 诊断性右心导管插入术和移植之间的中位时间为 8.7 年。 诊断和移植之间的肺血流动力学没有显着变化(表 1)。
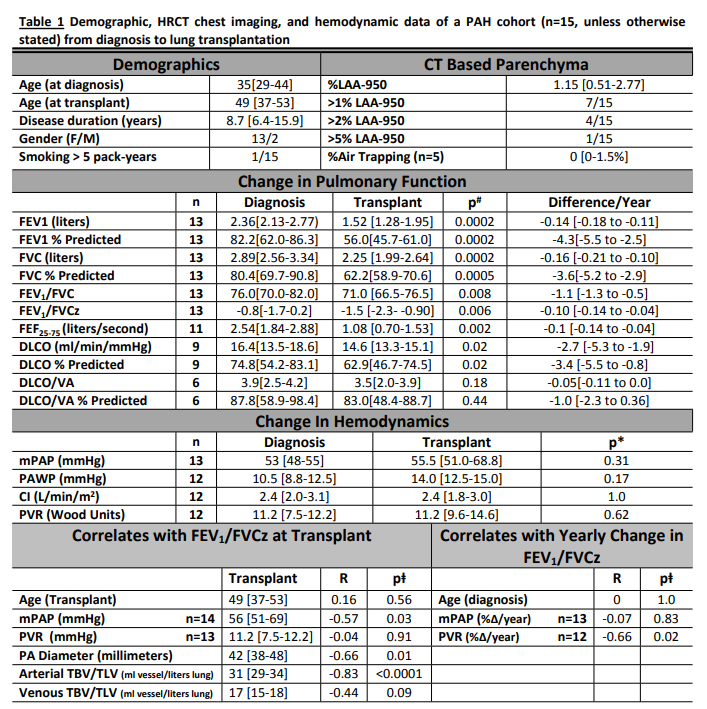
在肺移植时,大多数患者的 FEV1 (14/15) 和 FVC (13/15) 绝对值在第 5 个百分位数内,6/15 患者满足阻塞性肺病(OLD)的标准(图 1)。
从初始诊断到移植,绝对 FEV1以及FVC逐年显着下降;FEV1/FVC 比值从 76.0 [70.0-82.0] 显着下降至 71.0 [66.5-76.5],每年下降 1.1 [0.5-1.3]。同样,FEV1/FVCz 从-0.8 [-1.7 至 0.2] 显着下降至 -1.5 [-2.3 至 -0.90],每年下降 -0.10 [-0.14 至 -0.04]。因此,大多数患者从诊断到移植之间进展到更低(更负)的 FEV1/FVCz 百分位分类(图 1),这与阻塞性肺功能恶化一致。根据移植时的成像,没有肺气肿或空气滞留的证据(表 1),并且没有发现支持任何其他实质或气道疾病。
图1-左上图说明了绝对 FEV1 和 FVC 的变化;左下图说明了同一时间点之间每个受试者的 FEV1/FVCz 的演变;左下图说明每个 FEV1/FVCz 百分位数内的受试者数量,比较两个时间点,PAH 诊断和肺移植;右上图显示了两个有代表性的血管重建(受试者 #14 和 #12),并附有一个颜色图例,描述了基于横截面积从 0.8mm2(红色)到 100mm2(蓝色)的肺动脉尺寸范围;右下图显示与具有适度主肺动脉扩张和较高 FEV1/FVCz 的受试者相比,轴向截面在具有较低 FEV1/FVCz 的受试者中表现出相对严重的主肺动脉扩张。
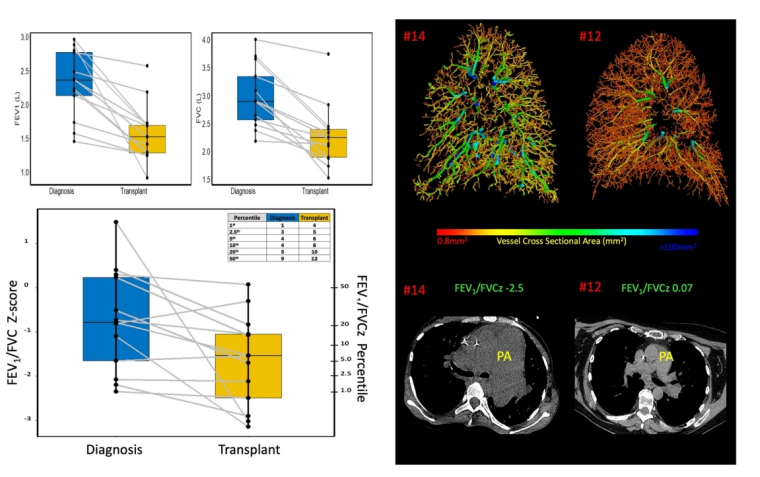
总之,该研究的分析表明,晚期 PAH 患者可能会表现出与胸部成像参数相关的进行性阻塞性生理,这些参数表明胸腔血容量增加,但没有空气滞留。这些发现支持扩大/充血的肺动脉直接或间接调节动态气道功能的假设。此外,建议将 PAH 添加到已知表现出限制性和阻塞性生理的现有呼吸系统疾病中。这种阻塞性生理机制是否会导致 PAH 中 V/Q 不匹配和气体交换的恶化,或者它是否对支气管扩张剂治疗有反应,仍有待确定。在未来的 PAH 临床试验中,可能需要考虑将连续肺功能作为终点。未来的研究需要确认阻塞生理学的演变并确定 PAH 的潜在机制。
原文出处:Rahaghi FN. Evolution of Obstructive Lung Function in Advanced Pulmonary Arterial Hypertension. Am J Respir Crit Care Med. 2021 Sep 23. doi: 10.1164/rccm.202105-1169LE. Epub ahead of print. PMID: 34555310.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#动脉高压#
36
#演变#
30
#阻塞#
41
#RCC#
39
学习了
63
学习了
51
👍 👍
77