Lancet oncol:3期随机试验| 二线FOLFOX化疗可显著改善晚期胆管癌预后
2021-04-03 MedSci原创 MedSci原创
FOLFOX(亚叶酸、氟尿嘧啶和奥沙利铂)化疗方案有望成为晚期胆管癌的标准化疗方案
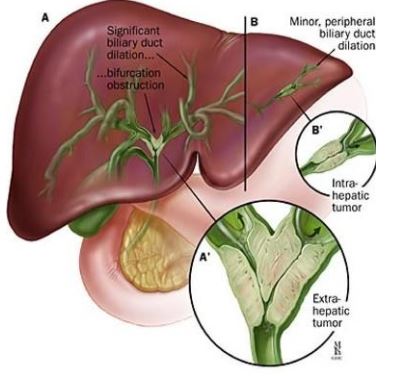
晚期胆管癌预后较差。顺铂和吉西他滨是标准的一线化疗方案,但尚无可靠的证据支持二线化疗。本研究旨在探索FOLFOX(亚叶酸、氟尿嘧啶和奥沙利铂)化疗方案用作二线治疗在晚期胆管癌中的治疗效益。
ABC-06临床试验是一项在英国20个地点开展的3期、开放标签的随机试验,招募年满18岁的组织学确诊的经一线顺铂和吉西他滨化疗后进展的局部晚期或转移性胆管癌(包括胆囊或壶腹癌)患者,按1:1随机分至两组,接受FOLFOX化疗和积极症状控制(ASC)或只接受ASC。主要终点是总存活期。
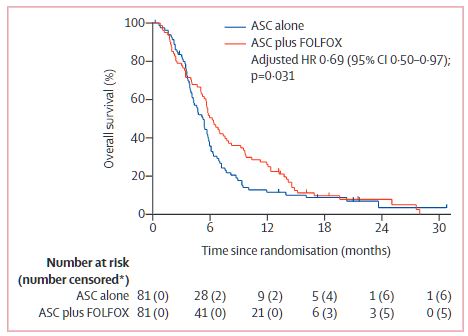
总存活率
2014年3月27日-2018年1月4日,共162位患者被随机分至ASC+FOLFOX组或单ASC组(各81位)。中位随访了21.7个月。与单ASC组相比,ASC+FOLFOX组的总存活期明显延长,中位总存活期分别为6.2个月 vs 5.3个月(校正风险比 0.69, 95% CI 0.50-0.97;p=0.031)。单ASC组的6个月总存活率为35.5%,12个月的总存活率为11.4%;而ASC+FOLFOX组的5个总存活率为50.6%,12个月的为25.9%。
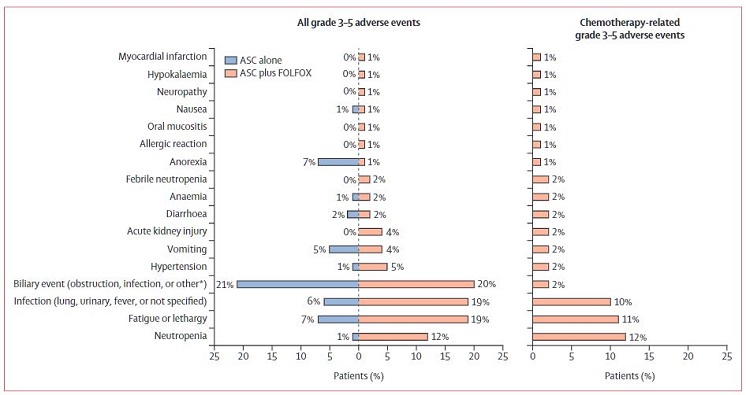
不良事件
单ASC组和ASC+FOLFOX组分别报告了42例(52%)和56例(69%)3-5级不良事件,包括3例化疗相关的死亡(分别死于感染、急性肾损伤和发热性中性粒细胞减少)。最常见的3-5级FOLFOX相关的不良事件是中性粒细胞减少(10例[12%])、疲劳或昏睡(9[11%])和感染(8[10%])。
总而言之,在ASC的基础上,予以FOLFOX可提高顺铂和吉西他滨治疗后进展的晚期胆管癌患者的中位总存活期(率),6个月和12个月的总存活率有临床意义的显著提高。据了解,该试验是第一个提供了晚期胆管癌患者可从二线FOLFOX化疗中潜在获益的可靠、高质量证据的前瞻性、随机试验。
原始出处:
Angela Lamarca, et al. Second-line FOLFOX chemotherapy versus active symptom control for advanced biliary tract cancer (ABC-06): a phase 3, open-label, randomised, controlled trial. The Lancet Oncology. March 30, 2021
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#Oncol#
38
FOLFOX方案作为晚期或转移性胆管癌的二线治疗,患者明显获益
58
#Lancet#
38
#FOLFOX#
40
#随机试验#
37
#胆管#
32
顶刊就是不一样,质量很高,内容精彩!学到很多
49
谢谢梅斯分享这么多精彩信息
62
高质量研究,读起来真爽,谢谢梅斯
43
OK
68