JCO:EGFR突变腺癌转化为非小细胞肺癌和其他神经内分泌肿瘤
2018-12-20 MedSci MedSci原创
大约3%至10%的EGFR突变的非小细胞肺癌(NSCLC)会转化为小细胞肺癌(SCLC),但其临床过程尚不明确。JCO近期发表了一篇文章研究这一问题。
大约3%至10%的EGFR突变的非小细胞肺癌(NSCLC)会转化为小细胞肺癌(SCLC),但其临床过程尚不明确。JCO近期发表了一篇文章研究这一问题。
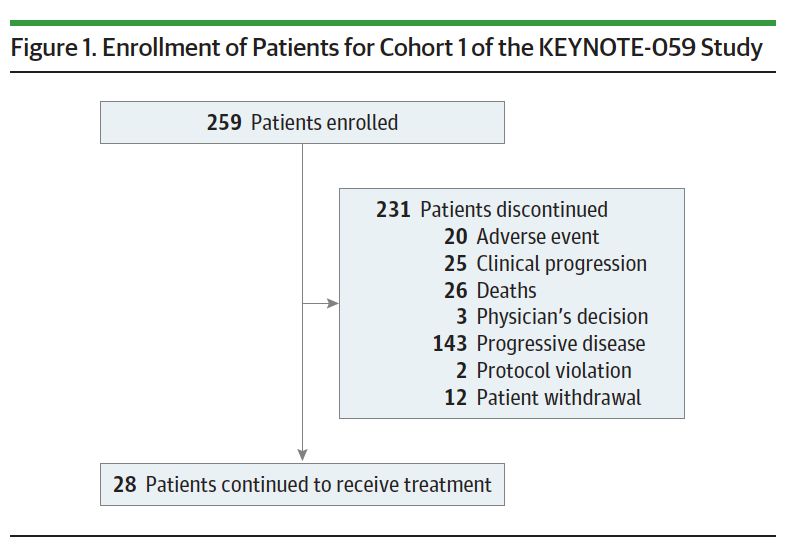
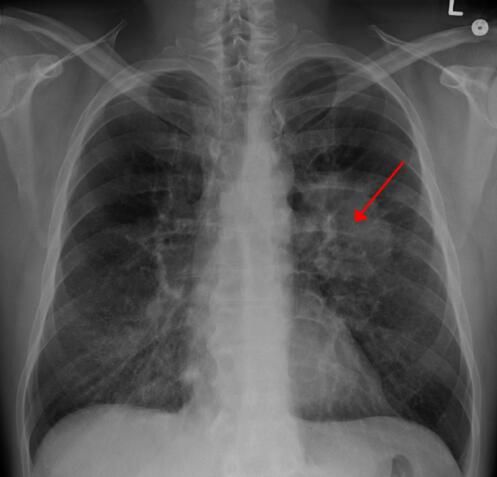
作者回顾性选取了患有EGFR-mutant SCLC和其他高级别神经内分泌癌的患者,分析了人口统计学,疾病特征和结果。研究共纳入67名患者--38名女性和29名男性; EGFR突变包括外显子19缺失(69%),L858R(25%)和其他(6%)。在肺癌初始诊断时,58名患者患有NSCLC,9名患者患有de novo SCLC或混合组织学类型。除了这9名患者外,所有患者在SCLC转化前都接受一种或多种EGFR酪氨酸激酶抑制剂治疗。转化的中位时间为17.8个月。转化后,铂-依托泊苷和紫杉烷均产生高反应率,但17名接受免疫治疗的患者均未出现反应。诊断后的中位总生存期为31.5个月,SCLC转化时的中位生存期为10.9个月。59例患者在首次出现SCLC时检测了组织分型。19例之前存在EGFR T790M阳性的患者中的15例在转化时为T790野生型。其他复发突变包括TP53,Rb1和PIK3CA。在一些病例中发现再次出现NSCLC克隆。转化CNS转移发生更为频繁。
原始出处:
Nicolas Marcoux, Scott N. Gettinger, et al. EGFR-Mutant Adenocarcinomas That Transform to Small-Cell Lung Cancer and Other Neuroendocrine Carcinomas: Clinical Outcomes. JCO. December 2018 doi: 10.1200/JCO.18.01585
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











学习了
29
#JCO#
29
#分泌#
35
#非小细胞#
29
#内分泌肿瘤#
29
#神经内分泌#
32
#GFR#
0