Journal of Cardiothoracic Surgery:900万人研究!冠脉搭桥术后30天再入院率及风险因素
2021-06-17 “E药世界”公众号 “E药世界”公众号
澳大利亚新南威尔士大学学者近日发表在《Journal of Cardiothoracic Surgery》杂志上的研究,量化了CABG手术后30天内的再入院率,分析了患者再入院原因及患者自身、医院相关
冠状动脉搭桥术(CABG)术后再入院,往往与不良预后、医疗开支的大幅增加显着相关。同时,术后30天再入院率也被认为是医疗护理质量的关键指标。
澳大利亚新南威尔士大学学者近日发表在《Journal of Cardiothoracic Surgery》杂志上的研究,量化了CABG手术后30天内的再入院率,分析了患者再入院原因及患者自身、医院相关因素。
研究者对PubMed、Embase数据库进行了系统性检索(截至2020年6月),以获取统计CABG术后再入院的观察性研究,使用随机效应荟萃分析来评估患者CABG术后30天再入院的发生率及相关因素。
研究最终纳入53项研究,共893 7457例CABG患者,合并后的CABG术后30天再入院率为12.9%(95% CI: 11.3–14.4%),常见原因包括:感染和脓毒症(6.9–28.6%),心律失常(4.5–26.7%),充血性心衰(5.8–15.7%),呼吸系统并发症(1–20%),胸腔积液(0.4–22.5%)。
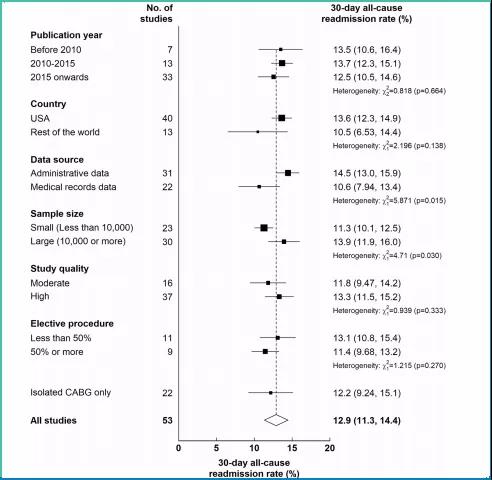
图片:依据不同研究特征对CABG术后30天再入院率进行亚组分析
另外,患者个人风险因素:
1. 年龄每增加10岁,风险增加12%;
2. 相比男性,女性风险相对高29%;
3. 相比白人,其他非白人种族风险高15%;
4. 当患者合并糖尿病、心衰、既往心梗、房颤、卒中或肥胖时,CABG术后30天再入院风险分别增高20%、25%、12%、33%、22%、10%。
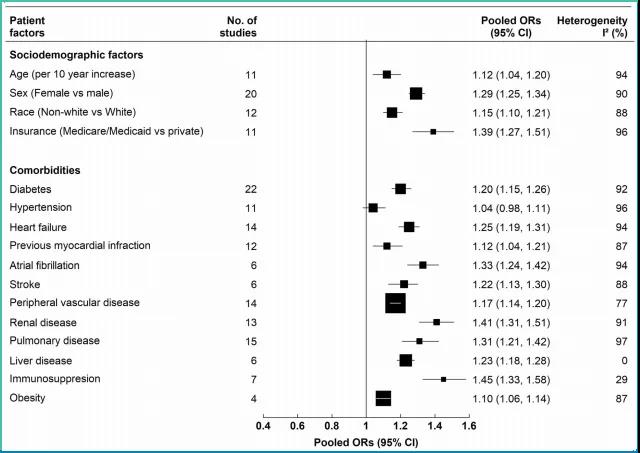
图片:患者自身因素与CABG术后30天再入院风险相关性的随机效应荟萃分析结果
医院相关因素有医院CABG手术量、相关医生人数、医院大小、医院水准质量及医院教学质量等。
该研究得出,几乎每8位冠状动脉搭桥术患者,就有1位会在术后30天内再入院,大多由非心脏原因引起。患者的再入院风险,与其人口学、临床特征有较大关联。而在医院层面的相关性,不同研究结论并不完全一致。
文献出处:
Md Shajedur Rahman Shawon, et al. Patient and hospital factors associated with 30-day readmissions after coronary artery bypass graft (CABG) surgery: a systematic review and meta-analysis. Journal of Cardiothoracic Surgery. Published: 10 June 2021.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#GER#
32
#冠脉搭桥术#
36
#30天#
44
#THORAC#
22
#surgery#
38
#搭桥#
0
#搭桥术#
38
#再入院率#
26
#冠脉搭桥#
30