PLoS One:黄体生成素/绒毛膜促性腺激素受体在前列腺癌细胞和患者中的新作用
2020-09-20 AlexYang MedSci原创
在肿瘤初始消退后,前列腺癌(PCa)细胞开始产生去势抵抗。肿瘤内类固醇从头合成可能是前列腺癌去势抵抗的生物学机制,但其调节机制尚不清楚。睾丸睾酮(T)的产生是由黄体生成素/绒毛膜促性腺激素受体(LHC
在肿瘤初始消退后,前列腺癌(PCa)细胞开始产生去势抵抗。肿瘤内类固醇从头合成可能是前列腺癌去势抵抗的生物学机制,但其调节机制尚不清楚。睾丸睾酮(T)的产生是由黄体生成素/绒毛膜促性腺激素受体(LHCGR)控制的。为了阐明LHCGR对前列腺癌发生的影响,来自哥本哈根大学等单位的科学家研究了LHCGR在前列腺癌中的存在和作用,以及血清中LHCGR是否对前列腺癌患者的预后有影响。
他们采用RT-PCR、WB、IHC、qPCR等方法检测了LHCGR在前列腺癌细胞系和前列腺组织中的表达,用LC-MS/MS在细胞系培养基中检测类固醇的产量,用qPCR检测类固醇合成酶的表达,并采用ELISA法测定了157例前列腺癌患者的血清LHCGR (sLHCGR)。
结果表明,他们在前列腺组织和前列腺癌细胞系中均发现了LHCGR的存在。在黄体生成素刺激下,LNCaP细胞增殖增加1.29倍(P = 0.007), PC-3细胞增殖增加1.33倍(P = 0.0007)。绒毛膜促性腺激素刺激可使DU145细胞增殖减少0.93倍(P = 0.05),但均未改变类固醇代谢物的分泌。与高浓度的sLHCGR相比,低浓度的sLHCGR与根治性前列腺切除术后更高风险的生化失败(HR = 3.05, P = 0.06)和更高的去势抵抗(HR = 6.92, P = 0.004)相关。LHCGR在PCa中表达,可能在PCa衍生细胞系中发挥生长调节作用。
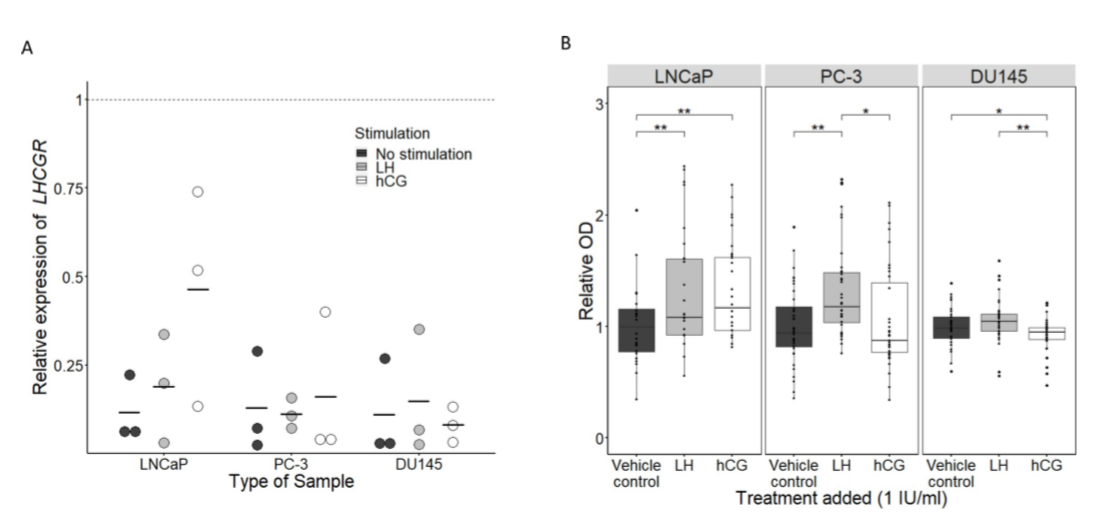
LH和hCG治疗对3种前列腺癌细胞系(LNCaP,PC-3和DU145)的影响
综上所述,本研究初步发现,sLHCGR在确定PCa患者复发风险方面具有潜在的预后作用,但需要在更大的队列中进行验证。
原始出处:
Stroomberg HV, Jørgensen A, Brasso K et al. Novel functions of the luteinizing hormone/chorionic gonadotropin receptor in prostate cancer cells and patients. PLoS One. 2020 Sep 3.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#Plos one#
32
#促性腺激素#
35
#新作用#
42
#癌细胞#
37
#前列腺癌细胞#
32
前列腺癌相关研究,学习了,谢谢梅斯
45