British Journal of Psychiatry:复杂型发展创伤对心理健康和认知功能的影响
2021-08-22 MedSci原创 MedSci原创
复杂型发展创伤是指儿童或青春期涉及多重人际威胁的创伤经历,例如反复虐待,是目前最普遍的创伤类型,也是当代社会最为重要的公共卫生问题。
复杂型发展创伤是指儿童或青春期涉及多重人际威胁的创伤经历,例如反复虐待,是目前最普遍的创伤类型,也是当代社会最为重要的公共卫生问题。

CCO
近日,发表在The British Journal of Psychiatry杂志的一项研究显示,遭受复杂型发展创伤的年轻人患有更为严重要的心理健康问题和认知障碍。该研究首次证明不同类型的创伤是否会带来相同的精神疾病风险。

在这项研究中,研究人员跟踪了 1994-1995 年出生于英格兰和威尔士的 2232 名儿童,并在18 岁时接受了复杂创伤暴露(例如反复虐待儿童)、其他非复杂创伤(例如车祸)的暴露以及心理健康问题和认知功能的评估。
结果发现,与未暴露于创伤的参与者和暴露于非复杂创伤的参与者相比,暴露于复杂型发展创伤的参与者在 18 岁时具有更严重的心理健康问题和更差的认知功能。
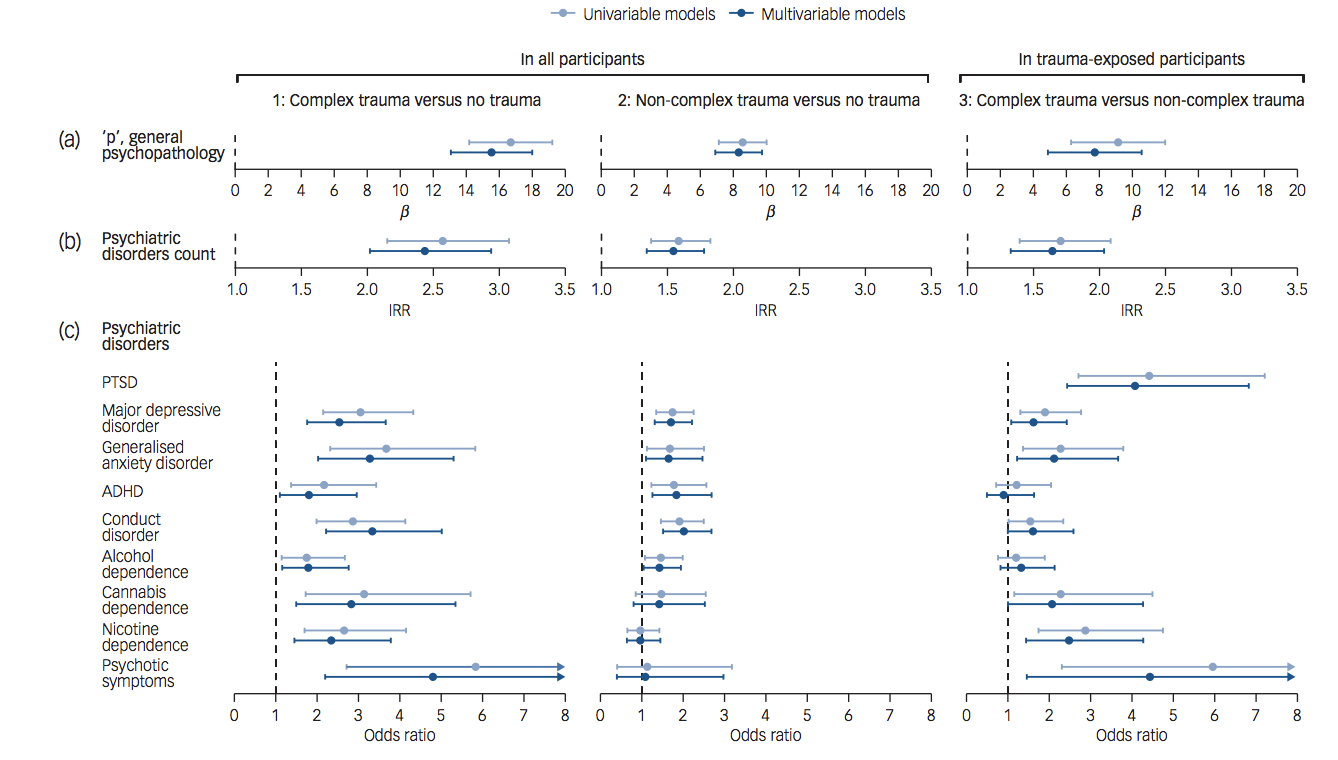
创伤暴露与心理病理学之间的关联,包括控制早期儿童的脆弱性。
同时,研究人员发现,在 5 岁时预测了未来复杂创伤暴露的风险,并在很大程度上解释了复杂型发展创伤暴露与认知障碍之间的关联,但不能解释与精神病理学的关联。
综上,,当前的研究和临床实践低估了与复杂创伤相关的精神病理学、认知缺陷和预先存在的脆弱性的严重程度。因此更好地了解遭受复杂创伤的人群的心理健康需求可以为开发新的、更有效的干预措施。
原始出处
Stephanie J. Lewis et al, Unravelling the contribution of complex trauma to psychopathology and cognitive deficits: a cohort study, The British Journal of Psychiatry (2021). DOI: 10.1192/bjp.2021.57
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#Psychiatry#
57
#创伤#
42
学习了。
78
很有帮助
63
学习了
74
学习了。
61