Lancet Neurology: 金刚烷胺、莫达非尼和哌甲酯治疗多发性硬化症疲劳的安全性和有效性:一项随机、交叉、双盲试验
2021-01-31 MedSci原创 MedSci原创
疲劳,定义为个人在日常活动中感觉到的身体或精神能量的主观缺乏,是多发性硬化症(MS)最常见和致残的症状之一,并且在患病期间的某个时间点影响超过75%的患者。
疲劳,定义为个人在日常活动中感觉到的身体或精神能量的主观缺乏,是多发性硬化症(MS)最常见和致残的症状之一,并且在患病期间的某个时间点影响超过75%的患者。疲劳对健康相关的生活质量有负面影响,超过50%的患者将其描述为疾病的最严重的症状。疲劳是一种主观症状,其很难与白天过度嗜睡或运动和认知疲劳区分开来。睡眠障碍、甲状腺功能不全和贫血也可加重疲劳的严重程度。
MS疲劳患者常伴有抑郁症,并且MS恶化可能加剧慢性疲劳。哌醋甲酯、莫达非尼和金刚烷胺是缓解MS患者疲劳的常用药物,然而支持其疗效的证据并不多见且相互矛盾。本文的研究的目标是比较这三种药物与安慰剂对MS相关疲劳患者的疗效。
在这项随机、双盲、安慰剂对照、四期交叉试验中,研究人员主要在美国的两个MS学术中心招募了报告疲劳且改良疲劳影响量表(MFIS)评分超过33分的MS患者。共141例受试者接受口服金刚烷胺(每天两次,最多100毫克)、莫达非尼(每天两次,最多100毫克)、哌醋甲酯(每天两次,最多10毫克)或安慰剂,每次服用6周。其中35名患者被分配到金刚烷胺、安慰剂、莫达非尼、哌甲酯序列;34名患者接受安慰剂、哌甲酯、金刚烷胺、莫达非尼序列;35例患者接受莫达非尼、金刚烷胺、哌甲酯、安慰剂序贯治疗;和37名患者服用哌甲酯、莫达非尼、安慰剂、金刚烷胺序列。所有患者依次接受所有四种研究药物,两种药物之间有两周的间隔期。本研究的主要疗效指标是在每个用药周期的第五周服用最高耐受剂量时测量的MFIS,同时使用线性混合效应回归模型进行分析。
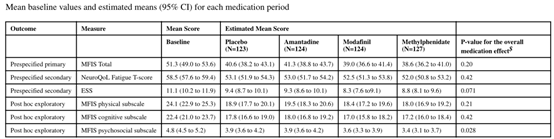
共有136受试者的数据可用于主要结果的意向治疗分析。基线时MFIS总分(95%CI)和最大耐受剂量的估计平均值如下:基线时51.3(49.0-53.6),安慰剂组40.6(38.2-43.1),金刚烷胺组41.3(38.8-43.7),莫达非尼组39.0(36.6-41.4),哌醋甲酯组38.6(36.2-41.0)。与安慰剂组[38名患者(31%)]相比,更高比例的受试者在服用金刚烷胺[49名患者(39%)]、莫达非尼[50名患者(40%)]和哌醋甲酯[51名患者(40%)]时报告了不良事件,包括服用金刚烷胺时出现肺栓塞和心肌炎,服用莫达非尼时出现需要住院治疗的MS恶化。
综上所述,金刚烷胺、莫达非尼和哌醋甲酯在改善MS疲劳方面并不优于安慰剂(通过有效的结果评估),并导致更频繁的不良事件。
Nourbakhsh, Bardia et al. Safety and efficacy of amantadine, modafinil, and methylphenidate for fatigue in multiple sclerosis: a randomised, placebo-controlled, crossover, double-blind trial. The Lancet Neurology, Volume 20, Issue 1, 38 - 48
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#Neurol#
29
#哌甲酯#
46
#多发性#
27
#硬化症#
35
#金刚烷胺#
44
#莫达非尼#
42
#Lancet#
27
#安全性和有效性#
22
#疲劳#
36
#双盲#
30