Mov Disord:DTI研究发现丘脑背内侧核游离水与帕金森病认知能力下降相关
2022-01-02 影像小生 MedSci原创
丘脑背内侧核 FW是一种有希望的早期帕金森病认知进展的生物标志物,有助于临床试验中识别认知保护疗法。FW是这些结果的可靠评估模式。
脑弥散张量成像(DTI)能反映早期帕金森病(PD)的认知变化,但尚未对基于弥散序列的游离水(FW)测量进行评估。基于弥散序列的FW评估已被证明比常规DTI 对PD患者黑质的纵向变化更敏感。FW对应体素中的水分子,它们不受细胞环境的阻碍或限制,因此来源于细胞外的水有病理证据支持FW反映组织萎缩和炎症。因此,FW水平越高,组织退化更严重。
Thomas Guttus等选择FW作为这些比较的主要结果成像评估方式。他们假设一个或多个主要ROI中FW的1年纵向变化与MoCA评分的1年和3年纵向变化呈负相关。这些发现将支持FW在这些ROI中作为认知进展的生物标志物。该研究结果发表在Mov Disord杂志。
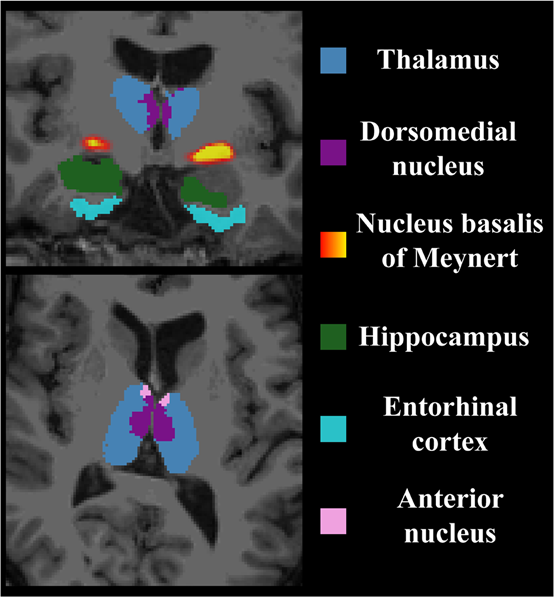
该研究评估丘脑的FW是否主要参与认知功能(即背内侧核和前核)、Meynert基底核(nbM)和海马是否与纵向认知功能下降相关,并区分早期帕金森病患者的基线认知状态。此外,探讨FW与常规DTI、FW校正DTI以及这些结果的体积评估的比较。
采用部分相关分析和ANCOVA方法对帕金森病进展标志物计划数据库中的影像数据和蒙特利尔认知评估(MoCA)评分进行分析。
自由水评估与帕金森病认知能力相关性的主要结果
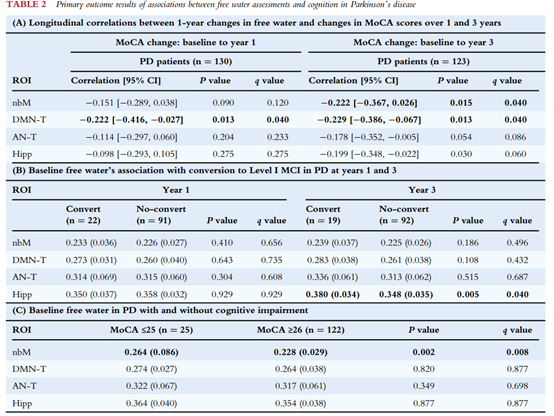
主要研究结果有:
1.丘脑DMN FW 1年的变化与MoCA 1年和3年的变化相关(偏相关系数=0.222,q = 0.040, n = 130; 偏相关系数=0.229, q = 0.040, n = 123; 基线平均PD持续时间= 6.85个月)。
2.nbM FW 1年的变化仅与MoCA 3年的变化相关(0.222,q = 0.040)。
3.基线海马FW与3年认知障碍相关(q = 0.040),基线nbM FW区分PD-正常认知(MoCA≥26)和PD-认知障碍(MoCA≤25) (q = 0.008)。
探索性比较显示FW是最可靠的评估方式。
丘脑背内侧核 FW是一种有希望的早期帕金森病认知进展的生物标志物,有助于临床试验中识别认知保护疗法。FW是这些结果的可靠评估模式。
原文出处
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#研究发现#
50
#DTI#
47
#Dis#
43
#Disord#
34
#认知能力下降#
54
#丘脑#
0
#丘脑#
33