JCO:3期TOURMALINE-MM1试验| 复发/难治性MM患者采用伊沙佐米-来那度胺-地塞米松治疗的总生存期终分析
2021-06-11 Nebula MedSci原创
具有不良预后因素的亚组患者可从ixazomib-Rd治疗中获得更大的OS效益
双盲、安慰剂为对照的3期TOURMALINE-MM1研究表明伊沙佐米-来那度胺-地塞米松(ixazomib-Rd)方案相比安慰剂-Rd能显著改善复发/难治性多发性骨髓瘤患者的无进展生存期。本文报告了该研究总生存期(OS)的最终分析结果。
在该试验中,患者被随机分至ixazomib-Rd组(360人)或安慰剂-Rd组(362人),并根据既往治疗次数(1次 vs 2/3次)、蛋白酶体抑制剂(PI)暴露史(有 vs 无)和疾病分期(I-II期 vs III期)分层。总生存期(OS)是关键的次要终点。
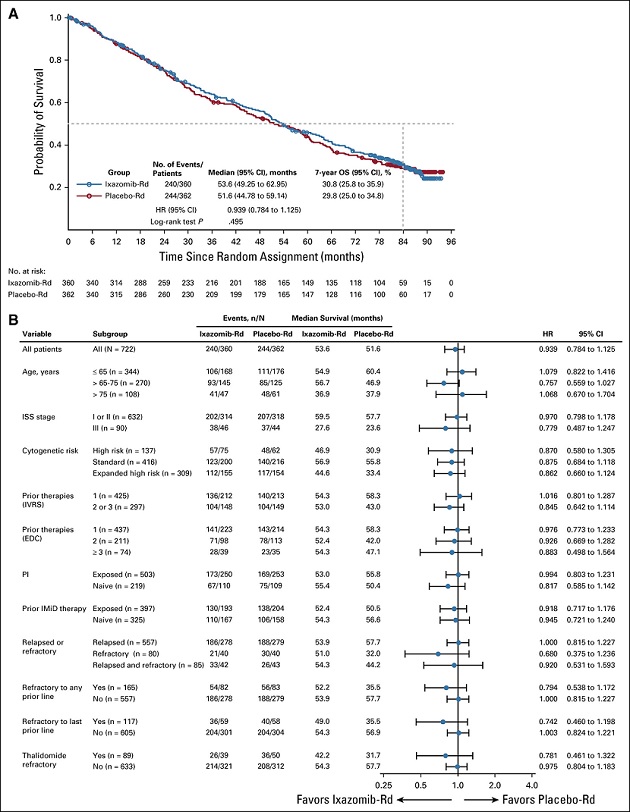
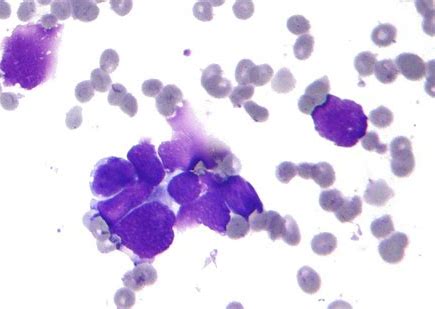
意向治疗人群和不同亚组的总生存期
中位随访85个月后,ixazomib-Rd组和安慰剂-Rd组的中位OS分别为53.6 vs 51.6个月(风险比[HR] 0.939,p=0.495)。在预定的亚组中观察到较低的风险比,提示ixazomib-Rd方案与安慰剂-Rd相比具有更大的OS效益:对任何治疗都不敏感(HR 0.794)、对最后一次治疗不敏感(0.742)、65-75岁(0.757)、III期(0.799)、既往治疗过2-3次(0.845)、高风险细胞遗传学(0.870)、高风险细胞遗传学和(或)1q21扩增(0.862)。
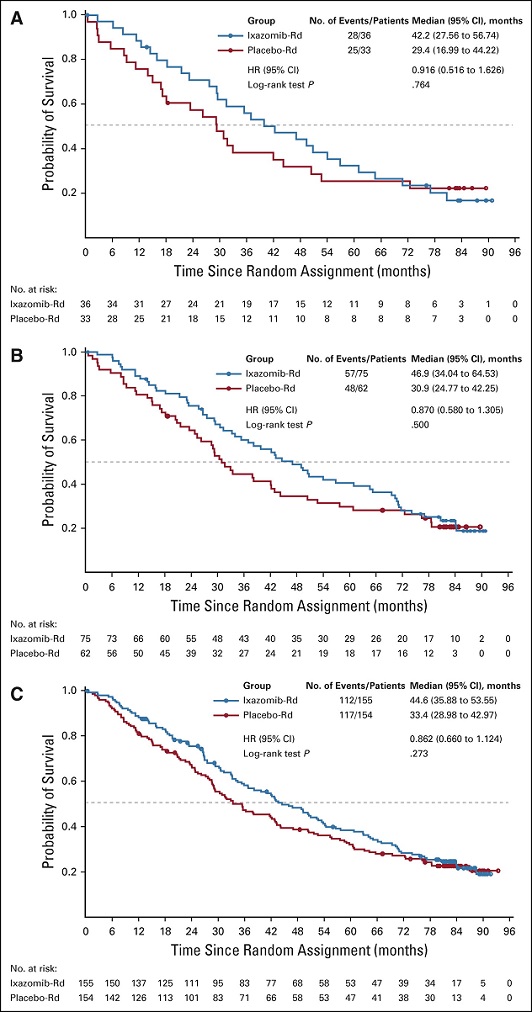
各种高风险细胞遗传学特征患者的总生存期
研究治疗后,ixazomib-Rd组 vs 安慰剂-Rd组分别有71.7% vs 69.9%的患者接受了其他抗癌治疗,其中分别有24.7% vs 33.9%的患者接受了达雷木单抗治疗,71.8% vs 76.9%的患者接受了PI治疗。
两组原发恶性肿瘤的新发率相近:ixazomib-Rd组(10.3%)、安慰剂-Rd组(11.9%)。无新发安全性问题。
综上,在本次分析中,ixazomib-Rd与安慰剂-Rd的无进展生存获益并未转化为具有统计学意义的OS获益。具有不良预后因素的亚组患者可从ixazomib-Rd治疗中获得更大的OS效益。
原始出处:
Paul G. Richardson, et al. Final Overall Survival Analysis of the TOURMALINE-MM1 Phase III Trial of Ixazomib, Lenalidomide, and Dexamethasone in Patients With Relapsed or Refractory Multiple Myeloma. Journal of Clinical Oncology. June 10, 2021
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











学习中
58
#JCO#
25
#生存期#
24
#总生存期#
34
#伊沙佐米#
33
#难治性#
23
在预定的亚组中观察到较低的风险比,提示ixazomib-Rd方案与安慰剂-Rd相比具有更大的OS效益。
60
在预定的亚组中观察到较低的风险比,提示ixazomib-Rd方案与安慰剂-Rd相比具有更大的OS效益
60