Angewandte Chemie:新型探针有助可视化检测胶质瘤标志物
2020-05-12 中国科学报 中国科学报
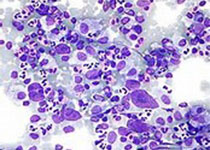
日前,中国科学院院士黄维与南京工业大学教授李林团队、新加坡国立大学科研人员合作,设计合成了一种新的双光子荧光探针,这将有助于未来临床上对人源胶质瘤标志物(单胺氧化酶 A,即 MAO-A)进行可视化精准
日前,中国科学院院士黄维与南京工业大学教授李林团队、新加坡国立大学科研人员合作,设计合成了一种新的双光子荧光探针,这将有助于未来临床上对人源胶质瘤标志物(单胺氧化酶 A,即 MAO-A)进行可视化精准检测。其成果以热点文章的形式发表于《德国应用化学》。
据介绍,人体内的神经递质代谢需要维持稳定的代谢平衡,如果单胺氧化酶的功能发生异常,会过多或过少地代谢神经递质,从而破坏生物体内神经递质的代谢平衡。所以单胺氧化酶与中枢神经系统疾病有密切联系,是中枢神经系统疾病研究中的重要生化标志物。
李林表示,基于各自代谢底物的不同,单胺氧化酶分为两种亚型(MAO-A 和 MAO-B),MAO-A 和 MAO-B 就像一对孪生兄弟,它们的构造极其相似,两者氨基酸序列相似率高达 70% 以上。它们的功能异常与不同疾病有关。在帕金森氏症中,MAO-B 作为生化标志物,而 MAO-A 则作为胶质瘤标志物。如何使设计的分子探针具有更高的特异性、灵敏性,来精确区分这两者,从而助力胶质瘤和帕金森氏症这两类疾病标志物的特异性检测,是一项具有挑战以及生物学意义的工作。
在前期研究中,研究团队已经设计出了针对 MAO-B 特异性双光子荧光探针 U1。在 U1 的结构基础上,日前,该课题组又设计了一种新的 MAO-A 特异性双光子荧光探针 F1,通过探针与 MAO-A 反应后的荧光信号来判断检测物中 MAO-A 的活性,从而有助于实现对人源胶质瘤的标志物 MAO-A 进行可视化精准检测。
据悉,这一新的 MAO-A 探针将为胶质瘤和帕金森氏症这两种机制完全不同的中枢神经系统疾病的相关性研究提供有力研究工具。
原始出处:
Haixiao Fang Hang Zhang, et al. Rational Design of a Two‐Photon Fluorogenic Probe for Visualizing Monoamine Oxidase?A Activity in Human Glioma Tissues. Angewandte Chemie, 2020, 59(19), 7536-7541.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#标志物#
40
#Angew#
50
#可视化#
37
#探针#
44