ESMO热点追踪之乳乳腺癌再启征程——PARP抑制剂展风采
2017-09-15 肿瘤资讯编辑部 肿瘤资讯
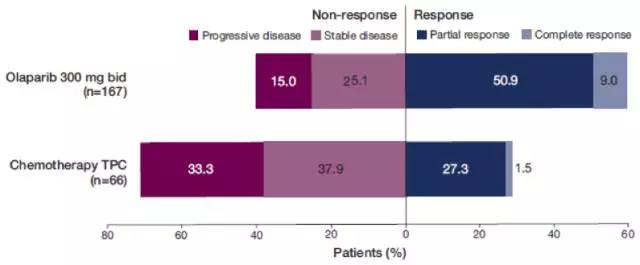
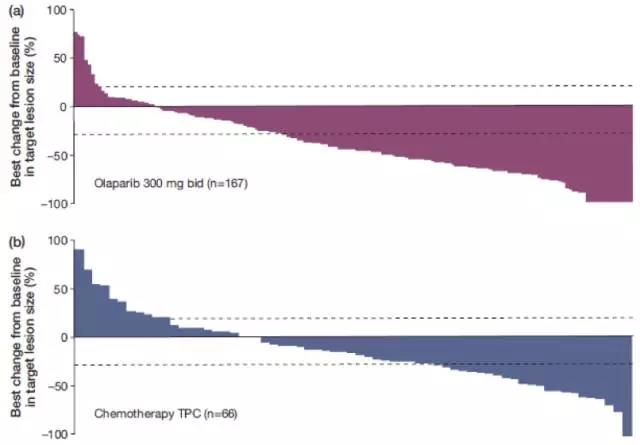
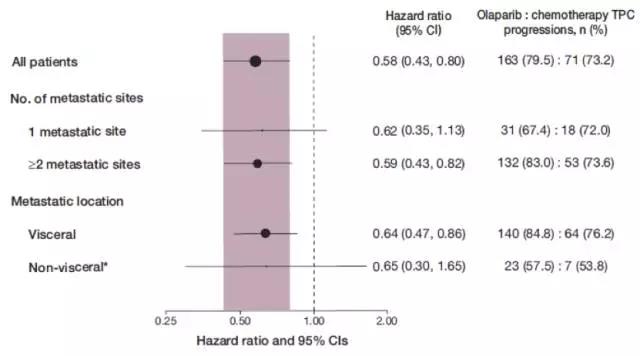
近年来,利用细胞固有的同源重组修复缺陷,通过“合成致死”理论杀死肿瘤细胞的概念成为肿瘤治疗领域的热点之一。其中研究最为成熟的药物是PARP抑制剂。而PARP抑制剂中率先取得成果的就是Olaparib(奥拉帕利)。在今年ESMO大会上,报道了多项关于Olaparib(奥拉帕利)在乳腺癌领域的研究。

本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#SMO#
36
#抑制剂#
23
学习了谢谢分享!!
72
不错的文章不错的文章
67
#ESMO#
19
#PARP#
30
感谢小编为我们准备了如此丰盛的精神大餐.同时也向作者致谢!认真学习了.点赞!
65
学习了.谢谢分享
56
.利用细胞固有的同源重组修复缺陷.通过[合成致死"理论杀死肿瘤细胞
60
学习并分享!!
23