JAMA子刊:SGLT2抑制剂与2型糖尿病和痛风发病率的关系
2021-11-23 MedSci原创 MedSci原创
与接受DPP4抑制剂的T2DM患者相比,接受SGLT2抑制剂的T2DM患者患痛风的风险更低。
钠-葡萄糖转运蛋白2 (SGLT2)抑制剂的使用是目前2型糖尿病(T2DM)患者的标准干预措施,对持续降低血尿酸水平具有良好的多效作用。然而,到目前为止,SGLT2抑制剂的使用与痛风的发生率之间的关联研究较少。本研究的目的是调查SGLT2抑制剂是否与T2DM患者痛风发生率较低相关。
这项队列研究回顾性分析了2016年5月1日至2018年12月31日期间台湾卫生机构数据库中所有发生T2DM的患者。作为对照,包括使用二肽基肽酶4(DPP4)抑制剂的患者。共评估了47905名接受SGLT2抑制剂的个体和183303名接受DPP4抑制剂的个体,以及47405对使用SGLT2抑制剂或DPP4抑制剂的患者进行了1:1倾向评分-匹配分析。数据分析于2021年4月1日至6月30日进行。
共有231208名2型糖尿病患者纳入人群,113812人(49.22%)为女性,平均年龄为61.53岁。SGLT2抑制剂使用者的总体痛风发病率为20.26/1000,DPP4抑制剂使用者为24.30/1000。当在倾向评分匹配人群中调整潜在危险因素时,与DPP4抑制剂相比,使用SGLT2抑制剂与痛风风险较低(HR,0.89;95%可信区间,0.820.96),尤其是对于接受达帕格列嗪的患者(HR,0.86;95%可信区间,0.78-0.95)。

2型糖尿病患者接受二肽基肽酶4 (DPP4)抑制剂和钠-葡萄糖共转运蛋白2 (SGLT2)抑制剂的痛风发生率
当使用ICD-9-CM或ICD-10-CM代码和痛风相关药物确定痛风诊断时,进行的敏感性分析也显示,使用SGLT2抑制剂的痛风发病率显著降低15%(HR,0.85;95%CI,0.74-0.97)。亚组分析表明,SGLT2抑制剂对T2DM患者降低痛风风险的益处在亚组间并无差异。
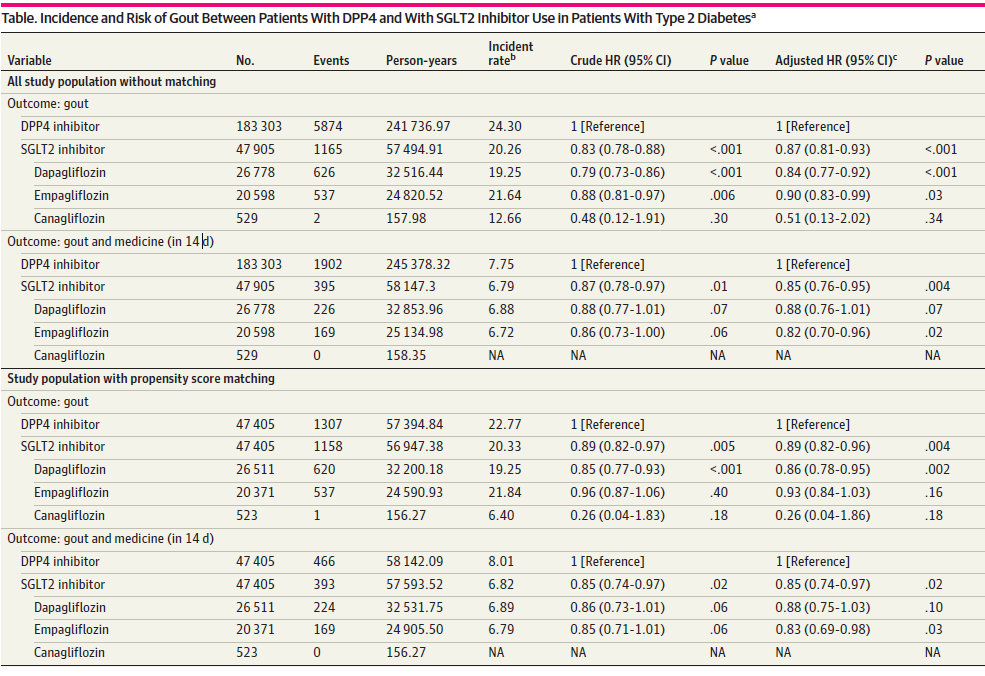
DPP4和SGLT2抑制剂在2型糖尿病患者中痛风的发生率和风险
这项研究的结果表明,与接受DPP4抑制剂的T2DM患者相比,接受SGLT2抑制剂的T2DM患者患痛风的风险更低。
参考文献:Chung M, Hung P, Hsiao P, et al. Association of Sodium-Glucose Transport Protein 2 Inhibitor Use for Type 2 Diabetes and Incidence of Gout in Taiwan. JAMA Netw Open. 2021;4(11):e2135353. doi:10.1001/jamanetworkopen.2021.35353
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言














#SGLT#
40
#发病率#
33
#抑制剂#
43
#2抑制剂#
42
#SGLT2#
34
厉害了
59
厉害了
60