Heart:非细菌性血栓性心内膜炎的人口统计学、诊断和结局
2022-05-14 MedSci原创 MedSci原创
非细菌性血栓性心内膜炎多发于女性,临床表现以栓塞并发症最为常见。总体而言,非细菌性血栓性心内膜炎患者预后较差,尤其是那些患有肺癌或转移性肿瘤的患者。
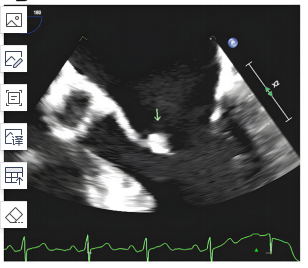
非细菌性血栓性心内膜炎是一种综合征,其特征是由于非感染性原因导致的心脏瓣膜增生和/或增厚。现在,基于超声心动图检查使得非细菌性血栓性心内膜炎的诊断成为可能。
近日,心脏病领域权威杂志Heart上发表了一篇研究文章,为了更好地描述这种疾病,研究人员对这些患者的流行病学、人口统计学、诊断和临床结局进行了回顾。
该研究纳入了2014年12月至2021年12月期间在梅奥诊所内所有诊断为非细菌性血栓性心内膜炎的成年人。非细菌性血栓性心内膜炎的诊断至少由两个专业的临床医生来确定,包括心脏病学、传染病学、风湿病学和肿瘤学专家。研究人员排除了血液培养阳性、感染性心内膜炎、心内膜炎培养阴性和研究授权未通过的患者。所有患者均随访1年。
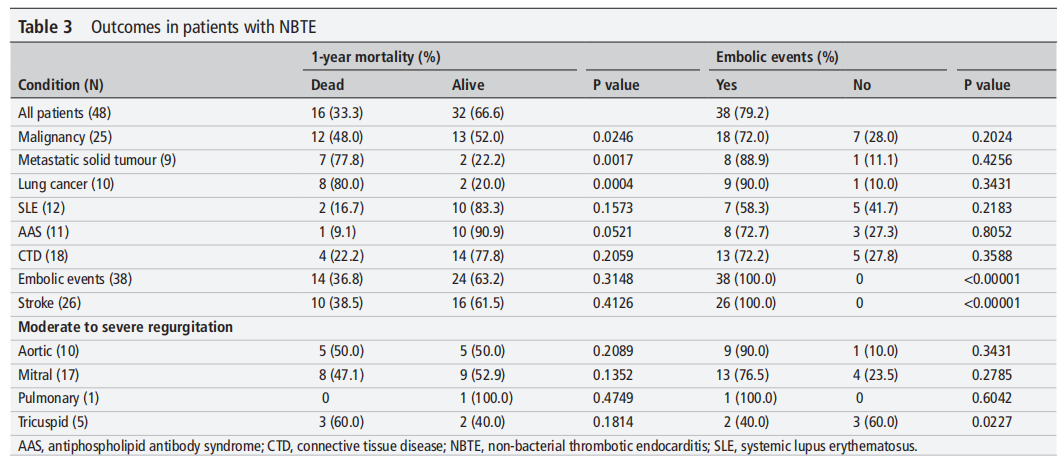
该研究共确定了48例患者,平均年龄为60.0±13.8岁,75%为女性。最常见的合并症是恶性肿瘤(52.1%)和结缔组织病(37.5%)。瓣膜异常包括41例(85.4%)为赘生物,43例(89.6%)为瓣膜增厚,26例(54.2%)为中度至重度返流。38例(79.2%)患者在诊断出非细菌性血栓性心内膜炎后1个月内发生栓塞事件(26例(54.2%)患者发生卒中),16例(33.3%)患者在诊断出非细菌性血栓性心内膜炎后1年内死亡。转移瘤和肺癌与患者1年全因死亡率相关(p=0.0017和p=0.0004)。
由此可见,非细菌性血栓性心内膜炎多发于女性,临床表现以栓塞并发症最为常见。总体而言,非细菌性血栓性心内膜炎患者预后较差,尤其是那些患有肺癌或转移性肿瘤的患者。考虑到非细菌性血栓性心内膜炎的发病率和死亡率,需要对其进行进一步的研究。
原始出处:
Juan A Quintero-Martinez.et al.Contemporary demographics, diagnostics and outcomes in non-bacterial thrombotic endocarditis.heart.2022.https://heart.bmj.com/content/early/2022/05/08/heartjnl-2022-320970
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#内膜#
53
#血栓性#
43
#心内膜炎#
56
#ART#
53
#统计学#
43
#HEART#
44
学习了
56