Br J Cancer:癌胚抗原CEA:转移性结直肠癌患者诱导治疗后疾病进展的标志物
2021-07-13 xiaozeng MedSci原创
癌胚抗原(Carcinoembryonic antigen,CEA)是一种参与细胞粘附的糖蛋白,通常在胎儿发育期间的胃肠组织中产生。
癌胚抗原(Carcinoembryonic antigen,CEA)是一种参与细胞粘附的糖蛋白,通常在胎儿发育期间的胃肠组织中产生。健康个体血液中CEA的血清水平通常较低(0–5 ng/ml),但在某些非肿瘤性疾病中可能会升高,包括炎症性肠病、肝炎、胰腺炎、肺部感染、吸烟者(很少超过10 ng/ml),以及胃肠道癌、肺癌和乳腺癌患者。
尽管约三分之二的结直肠癌(CRC)患者的 CEA 升高,但由于其敏感性和特异性较低,国际指南不建议将其用作筛查或诊断工具。
在转移性CRC(mCRC)中,血清CEA水平的变化可与影像学一起用于监测患者对全身治疗的反应。特别的是,既往的一系列回顾性研究显示,CEA的变异与患者的化疗反应之间存在着相关性,说明其或可预测疾病的进展(PD),以及在避免CT扫描方面的作用。
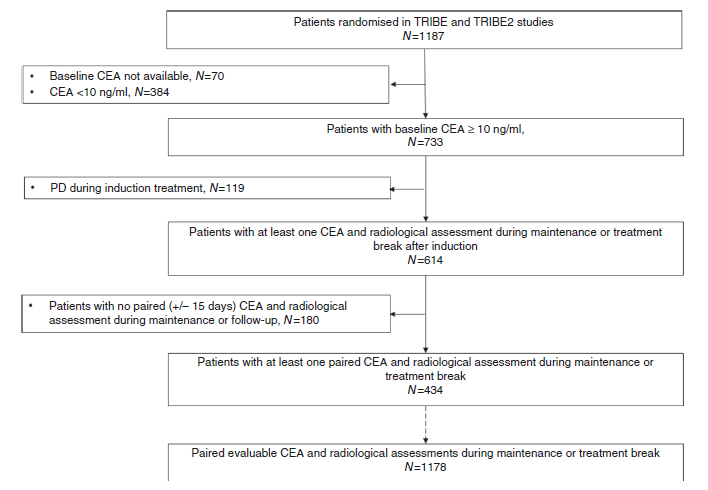
该研究汇集了TRIBE和TRIBE2研究中基线CEA≥10 ng/mL的患者的数据,旨在确定CEA升高百分比阈值,以预测诱导治疗结束后患者的疾病进展。
研究流程图
结果显示,该研究共包括了来自434名患者的1178次CEA水平和放射学数据。根据ROC曲线确定的最佳临界值显示,CEA从最低点增加至少120%的程度可区分疾病的进展与否,敏感性为74%,特异性为78%,92%的放射学评估中未出现PD且能够避免67%的CT扫描监测。
然而,在26%的病例中,120%CEA阈值并未检测到影像学PD。为改善这个问题,研究人员通过基于最佳灵敏度临界值评估了不同的临床相关阈值。因此,在使用从最低点开始的任何CEA升高作为阈值,检测的灵敏度增加到 93%,仅7%的患者未检测到影像学PD。
ROC曲线分析
总而言之,该研究结果揭示,在基线CEA≥10 ng/mL的mCRC中,CEA的水平可以准确的预测一线诱导治疗结束后患者的疾病进展与否。
原始出处:
Moretto, R., Rossini, D., Conca, V. et al. CEA increase as a marker of disease progression after first-line induction therapy in metastatic colorectal cancer patients. A pooled analysis of TRIBE and TRIBE2 studies. Br J Cancer (12 July 2021).
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#标志物#
25
#疾病进展#
32
#转移性#
29
#癌胚抗原#
38
#结直肠#
35
#CEA#
0
#抗原#
26