1. NEJM:新冠病毒12月中旬就已发现人传人
自2019年12月起,武汉发现了越来越多的新型冠状病毒(SARS-CoV-2)感染肺炎(下文称新冠肺炎)病例。2019年12月29日,当地医院运用“不明原因肺炎”监测机制,发现了最早报告的4个病例,这4例均与华南海鲜批发市场相关。上述监测机制是在2003年暴发严重急性呼吸系统综合征(SARS)疫情后建立,目的是尽早发现新型病原体(如SARS-CoV-2)。
随后我国其他城市和全世界十几个国家都发现了感染病例。中国疾病控制和预防中心(CDC)和当地CDC工作人员构成联合团队对武汉市最早的425例实验室确诊病例的数据进行了分析,从而描述新冠肺炎的流行病学特征和传播动力学。结果于1月30日在线发表在《新英格兰医学杂志》(NEJM)上。
Early Transmission Dynamics in Wuhan, China, of Novel Coronavirus-Infected Pneumonia. DOI: 10.1056/NEJMoa2001316
研究收集经实验室确诊的新冠肺炎病例的人口统计学特征、暴露史和疾病时间线的信息,描述了病例特征,并估计了关键流行病学延迟时间分布情况。在呈指数增长的初期,研究人员估计了传染病倍增时间和基本再生数。
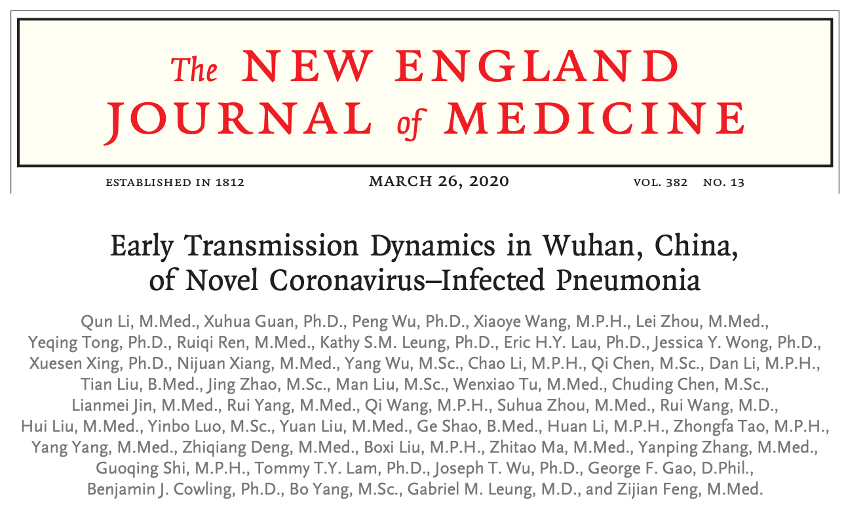
研究结果显示,在最早的425例新冠肺炎确诊患者中,中位年龄为59岁,56%为男性。在2020年1月1日前发病的病例中,大部分(55%)与华南海鲜批发市场相关,而在此后发病的病例中,仅8.6%与华南海鲜批发市场相关。平均潜伏期为5.2日(95%CI,4.1~7.0),潜伏期分布情况的第95百分位数为12.5日。在初期,倍增时间为7.4日。由一人传至另一人的平均间隔时间为7.5日(95% CI,5.3~19),基本再生数估计为2.2(95% CI,1.4~3.9)。
图A潜伏期的估计分布情况;图B.由一人传至另一人的间隔时间的估计分布情况;图C发病至首次就诊的间隔时间估计分布情况;图D发病至住院的间隔时间的估计分布情况。
研究表明,自2019年12月中旬以来,密切接触者之间已发生人际传播,并在此后一个月内逐渐播散。
2. JAMA:腭舌手术治疗中重度阻塞性睡眠呼吸暂停症成年患者
阻塞性睡眠呼吸暂停(OSA)是一种以睡眠打鼾伴呼吸暂停和日间思睡为主要临床表现的睡眠呼吸疾病,如果不及时治疗,会带来许多不良影响,包括白天嗜睡、生活质量下降、心血管疾病发病率和死亡率增加,许多OSA患者接受辅助治疗后效果不显著。
睡眠呼吸暂停多级手术(SAMS)试验是一项标准化手术程序的随机临床试验,该试验可减轻患有中度或重度症状性OSA且常规器械治疗失败的成年患者的舌后阻塞情况。手术在改善OSA方面比持续进行的医学治疗更为有效。腭舌联合手术是SAMS其中之一。
澳大利亚弗林德斯大学医学院Richard教授团队探究了腭舌联合手术对OSA常规治疗失败患者的疗效。
doi:10.1001/jama.2020.14265
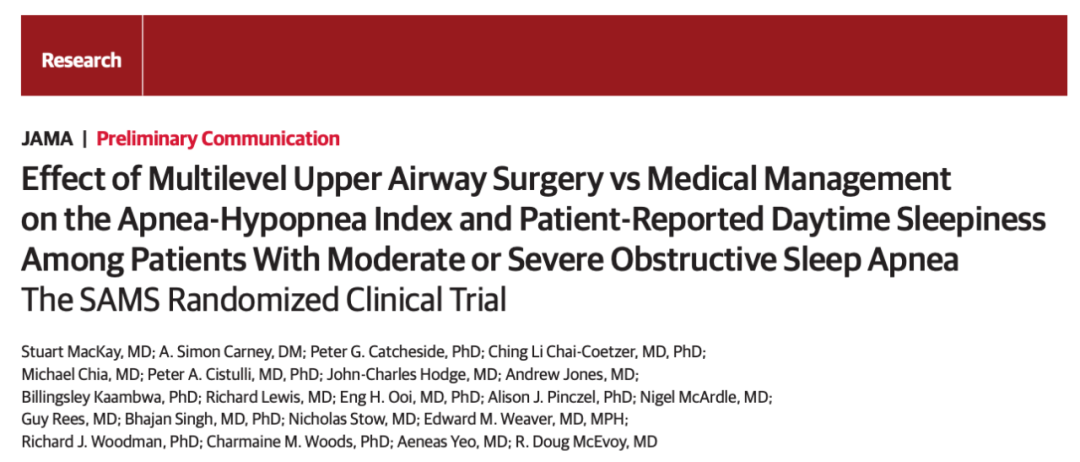
在该研究中,纳入的患者均为常规治疗失败以及症状性中或重度OSA患者,随机接受多次腭舌手术(改良悬雍垂腭咽成形术和微创舌体积缩小术)或常规医疗(例如,改善睡眠姿势或减肥)。研究的主要结果为睡眠呼吸暂停低通气指数(AHI;即呼吸暂停和低通气事件的次数/h;15-30表示中度OSA,>30表示重度OSA)和Epworth嗜睡评估(ESS;范围0-24;>10表示病理性嗜睡)。
上呼吸道手术与持续药物治疗OSA患者的影响研究中的AHI和ESS结果
手术组在基线检查时的平均ESS得分为12.4,6个月时为5.3;常规医疗组基线检查时的平均ESS为11.1,6个月时为10.5(6个月时,平均基线调整组间差异-6.7)。
研究表明,对于常规治疗失败的中、重度阻塞性睡眠呼吸暂停症患者,接受悬雍垂腭咽成形术和微创舌体积缩小术可减少呼吸暂停和低通气事件的发生,改善患者嗜睡症状。
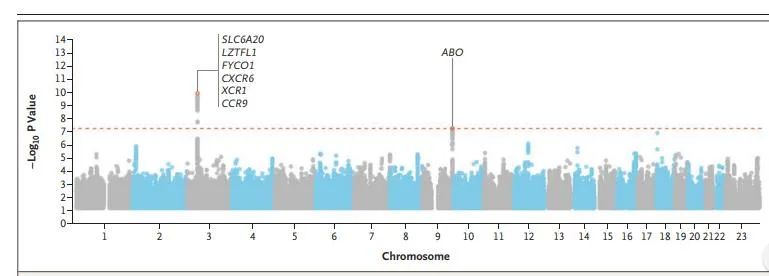
3. Am J Respir Crit Care Med:CHRNA5 / 3区域作为气流阻塞的遗传危险因素具有重要作用
慢性阻塞性肺疾病(COPD)是全球第三大死亡原因。根据肺活量测定法将COPD定义为在给予支气管扩张剂后不能完全逆转的气流阻塞。气流阻塞诊断需要FEV1及其与FVC的比值(FEV1/FVC)均小于各自的正常下限(FVC是对最大深度呼吸后可以强行呼吸的最大空气量的度量,FEV1是一秒钟内从肺部排出的空气量)。此前,医学界已确定全基因组关联研究(GWAS)影响肺功能的基因座,但已知影响COPD的基因较少。
为了一探究竟,荷兰鹿特丹大学教授Bruno H Stricker基于先前的人群家庭研究和病例对照研究进行了一项GWAS荟萃分析,以分析气流阻塞(气流阻塞是通过肺活量测定法评估的COPD的关键病理生理特征)。结果发表在AMERICAN JOURNAL OF RESPIRATORY AND CRITICAL CARE MEDICINE杂志上。
Genome-Wide Association Studies Identify CHRNA5/3 and HTR4 in the Development of Airflow Obstruction. doi: 10.1164/rccm.201202-0366OC
研究分析发现,在染色体15q25.1上有一个区域在有吸烟史人群中有全基因组意义,其中包括AGPHD1、IREB2和CHRNA5/CHRNA3基因,并且该区域在从未吸烟者中也有适度关联。
研究结果显示,基因表达研究证实CHRNA5/3存在于肺部、气道平滑肌和支气管上皮细胞中。除了15q染色体区域外,之前与FEV1/FVC相关的基因HTR4的单核苷酸多态性在吸烟者中也具有全基因组统计意义。
研究结果表明CHRNA5 / 3区域作为气流阻塞的遗传危险因素具有重要作用,该因素可能与吸烟无关,并提示HTR4基因也可能是导致气流阻塞的病因之一。
4. Lancet:首度公开新冠肺炎死亡危险因素
3月9日,由中日友好医院曹彬团队领衔完成,北京协和医学院、中日友好医院、武汉金银潭医院、清华大学医学院等机构联合在《柳叶刀》(Lancet)在线发表的回顾性队列研究。该研究首度公开新冠肺炎死亡危险因素。
Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study.
DOI: 10.1016/S0140-6736(20)30566-3
这项研究涵盖了191例患者(武汉金银潭医院135例,武汉肺科医院56例),其中137例出院,54例死亡。
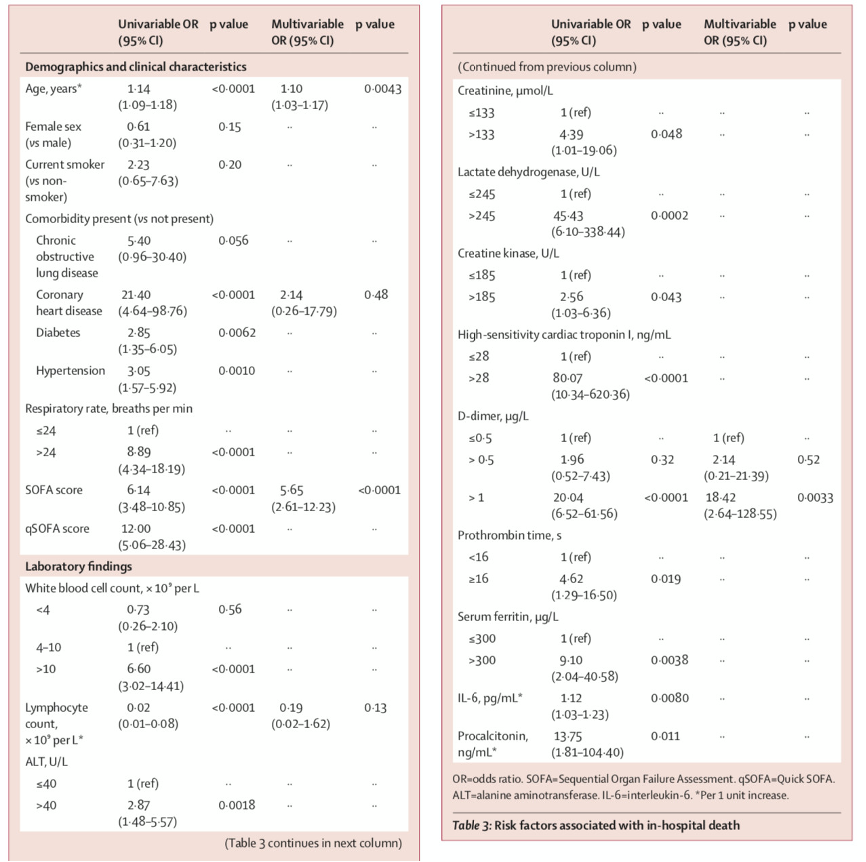
院内死亡相关危险因素
研究结果发现,对于年龄较大、d-二聚体水平大于1μg/ L、入院时SOFA评分较高与院内死亡几率呈高相关。除了这几个独立危险因素外,在重症新冠肺炎患者中,还有一些临床特点也预示着病人的预后差,诸如淋巴细胞减低、IL-6过度升高以及铁蛋白过度升高。
此外,该研究首次发现一半以上的患者患有脓毒症,在患者入院时未检测到细菌病原体感染的情况下,患者已经出现了脓毒症。该研究提示,在之后的新冠肺炎发病机制研究中,基础医学研究者应把研究重点放在病毒感染引起的病毒性脓毒症的发病机制上,这对于患者隔离决策和抗病毒治疗时间的指导均具有重要意义。在重感染患者中,延长的病毒脱落与死亡结果相关,病毒的复制和排毒时间与患者的预后直接相关,想要改善患者预后,必须采取及时有效的抗病毒治疗措施。
5.NEJM:确定电子烟中导致相关性肺损伤的成分
电子烟是称为电子尼古丁传送系统的典型形式,为吸入目的汽化含有尼古丁的液体。自2019年以来,美国不断传出电子烟导致使用者出现肺炎甚至死亡的病毒,今年2月中旬,美国CDC报告了全美2800多例需要住院治疗的电子烟使用相关肺损伤(EVALI),影响之大。因此美国CDC团队在NEJM上发表了一项聚焦EVALI的研究,确定当前导致EVALI爆发的病原体。
Vitamin E Acetate in Bronchoalveolar-Lavage Fluid Associated with EVALI.
DOI: 10.1056/NEJMoa1916433
研究从患有EVALI的患者中检测支气管肺泡灌洗液(BAL)中的有毒物质,进行同位素稀释质谱分析,以测量几种医学界公认的有毒物质:维生素e醋酸酯,植物油,中链甘油三酸酯油,椰子油,石油馏出物和稀释剂萜烯。
分析结果显示,在EVALI患者的BAL液中检出了维生素E醋酸酯,另外,在BAL液中也可检测到四氢大麻酚(THC)和尼古丁以及它们的代谢物,THC是大麻中的活性成分,通常被用在违法产品中,维生素E醋酸酯被用作THC的电子液体的切割剂。
该研究证实含四氢大麻酚产品电子烟中添加维生素E醋酸酯导致相关性肺损伤,导致肺部的表面活性物质“无法提供维持呼吸所必须的表面张力。另外,加热维生素E醋酸酯可以产生致癌的烯烃和苯,而这些物质在医学领域被公认为对人体产生有害影响。
6. Am J Respir Crit Care Med:奥马利珠单抗可抑制阿司匹林超敏反应
阿司匹林加剧呼吸道疾病(AERD)的特征在于重度哮喘、阿司匹林超敏反应和其他非甾体抗炎药、慢性鼻窦炎与鼻息肉病和半胱氨酰白三烯。尽管非特异性AERD很常见,但有一部分患者会出现血清总IgE水平升高。
在AERD中,阿司匹林超敏反应通常是终生的,意外暴露于非甾体抗炎药会导致后续危及生命的哮喘发作。系统性皮质类固醇治疗可部分减轻AERD中阿司匹林引起的气道症状,但不能完全抑制终生的阿司匹林超敏反应。除了阿司匹林脱敏外,没有一种治疗方法能完全抑制阿司匹林超敏反应。因此,在接触非甾体类抗炎药物后,确定能强烈抑制超敏反应的药物非常重要。
奥马利珠单抗是一种人源化重组单克隆抗IgE抗体,可选择性地与IgE恒定区结合,阻断游离IgE与IgE受体的结合。以往的研究表明,奥马珠单抗治疗可以抑制阿斯匹林超敏反应,但目前尚未有随机试验探究奥马珠单抗对AERD、阿司匹林超敏反应和尿白三烯E4(LTE4)过量生产的功效。此外,仍不清楚在开始奥马珠单抗治疗后的哪个时间点对AERD患者进行临床疗效观察。
来自日本湘南镰仓综合医院免疫学和过敏学中心团队在呼吸顶刊American Journal of Respiratory and Critical Care Medicine发表了一篇研究,旨在评估患者在口服阿司匹林治疗期间,奥马利珠单抗对阿司匹林超敏反应、LTE4过量产生和AERD的疗效。
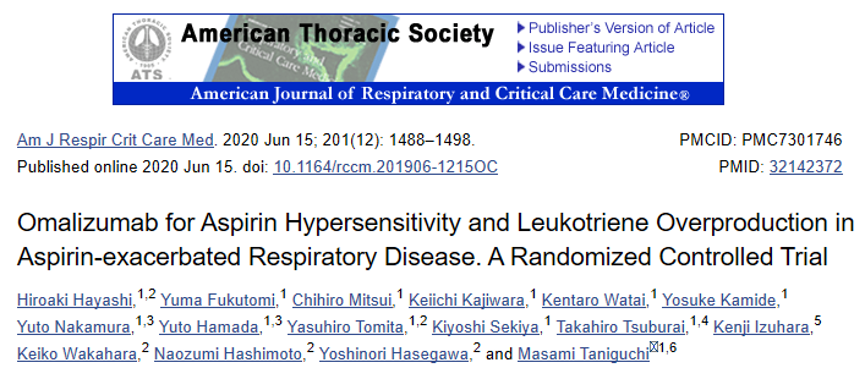
Omalizumab for Aspirin Hypersensitivity and Leukotriene Overproduction in Aspirin-exacerbated Respiratory Disease. A Randomized Controlled Trial. doi: 10.1164/rccm.201906-1215OC
研究人员进行了一项双盲、随机、交叉、安慰剂对照的单中心研究。将AERD特应性患者随机分配,分别接受奥马利珠单抗或安慰剂治疗3个月,然后进行>18周的冲洗期(交叉设计)。主要终点是口服阿司匹林试验期间,意向治疗人群的LTE4浓度对数下面积水平与时间曲线的差异。并测量了LTE4和肥大细胞的主要环氧合酶产物(tetranor-PGDM)。
(A和B)安慰剂和奥马珠单抗LTE 4(A)和tetranor-PGDM(B)浓度水平不同。
研究结果显示,口服阿司匹林试验期间LTE4浓度与时间曲线的对数下面积水平在奥马珠单抗阶段显著低于安慰剂阶段。
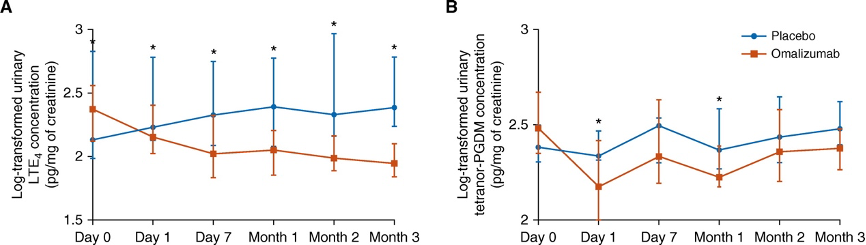
安慰剂和奥马利珠单抗各阶段的尿液和血液生物标志物的差别
此外,研究人员表示,在奥马珠单抗治疗的7天内,外周嗜酸性粒细胞计数和血清骨膜素水平被显着抑制,这些结果表明,奥马利珠单抗可以在24小时内开始有效抑制AERD中严重的嗜酸性气道炎症和肥大细胞活化,并有可能在3个月内改善阿司匹林超敏反应。
该研究结果表明,奥马利珠单抗治疗抑制了口服阿司匹林治疗过程中LTE4的过量产生和上/下呼吸道症状,同时抑制阿司匹林超敏反应。
7. JAMA:2020年哮喘指南更新
由于频繁的发病率和死亡率,哮喘成为世界范围内的主要公共卫生问题之一。哮喘指南(GINA)于1991年由美国国家心脏、肺和血液研究所首次发布,并于2007年更新。今年,该专家小组再次更新了哮喘指南发表在JAMA杂志上,还应“新型冠状病毒肺炎(Covid-19)大流行”之景,提出了疫情下哮喘管理治疗的临时指导意见。
JAMA
GINA2020更新要点如下:
1. 建议哮喘患者继续使用其正在使用的处方药物,尤其是要继续照常规范使用吸入糖皮质激素(ICS)和口服糖皮质激素(OCS)等。突然停止ICS治疗会导致潜在风险,包括哮喘加重、恶化等;对于重症哮喘患者,应继续使用生物治疗,避免突然停用OCS。
2. 轻度哮喘的治疗管理新增支持证据,所有成人和青少年轻度哮喘患者都应使用含有低剂量ICS的控制药物治疗方案,以减少发作风险,并且基于安全性考虑,不再建议单独使用短效β2受体激动剂(SABA)治疗。
3. 轻度哮喘患者按需使用ICS-福莫特罗时不需要进行炎症表型分析;按需使用ICS-福莫特罗在降低风险和控制症状方面的益处与基线特性无关。
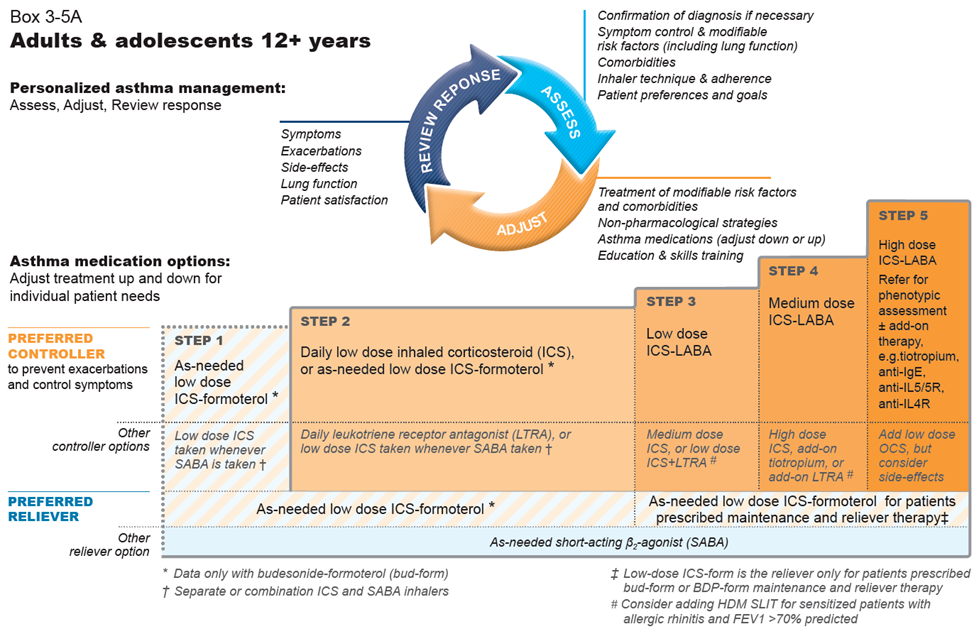
2020 GINA 哮喘阶梯治疗方案(成人及青少年)
4. 警惕孟鲁司特钠的不良反应
FDA已于2020年3月对孟鲁司特钠进行了黑框警告,提醒警惕其引起的包括自杀在内的严重神经精神不良反应。
5. 哮喘发病影响因素新的证据表明,全球13%的儿童哮喘可能与交通导致的空气污染有关,肥胖也可能是哮喘发病的危险因素。
6. 儿童哮喘管理
2020年增加的新证据包括一项系统综述表明,包括哮喘自我管理在内的以学校为基础的治疗方案减少了患哮喘儿童的急诊次数、住院次数和活动减少的天数。每日吸入皮质激素比孟鲁司特钠等白三烯受体拮抗剂(LTRA)可以更有效地控制症状和减轻病情。
7. 哮喘合并COPD章节被重写
哮喘合并慢性阻塞性肺疾病(COPD),兼具哮喘和COPD特征,临床上常见。GINA 2020对这部分进行了重写,关注临床认知和安全的初始治疗,添加了新的摘要图。这部分的重点是对初级保健和普通临床医生的建议。有研究证据表明,有哮喘和COPD特征的患者应使用含ICS的药物治疗方案,与单独使用长效支气管扩张剂相比,含ICS的治疗方案可以降低其住院和死亡风险。
对于哮喘,尽管尚无治愈方法或确立的预防手段,但仍可获得有效的治疗方法,此次《 2020年哮喘指南更新》中的建议将改善哮喘患者的健康。

以上研究是梅斯医学整理的呼吸领域一些重大突破性研究,当然2020年还有很多很多值回顾的亮点研究,欢迎留言补充哦~
相信在即将到来的2021年还会有更多精彩的研究,让我们拭目以待!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







学习
71
感谢分享
102
学习了!
88
#梅斯#
45
#研究进展#
46
好的咖啡
89
太好了
98
个免费
73
漂亮
30
谢谢,学习了
41