JAMA:美国儿童扁桃体切除术后死亡风险及相关因素研究
2022-06-23 zhangfan MedSci原创
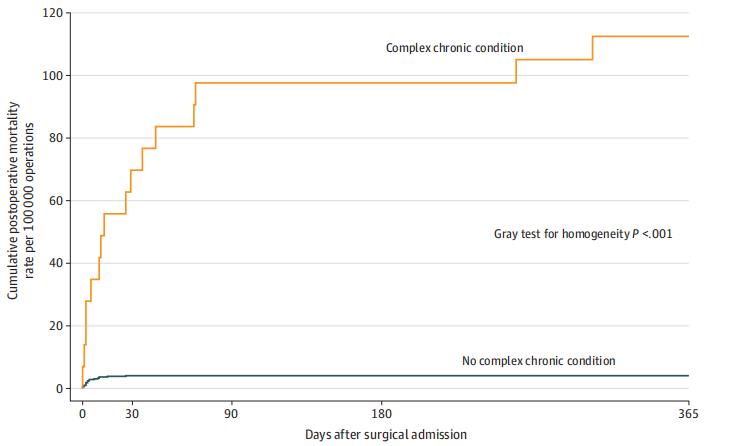
美国扁桃体切除患儿术后总死亡率为每10万分之7,但对于患有复杂慢性疾病的儿童,其风险高达每10万分之117。

统计称,2006年美国儿童扁桃体切除术手术超过50万例,2019年数据也高达37.7万例,但相关的术后患儿死亡率数据尚不充分,估计每10万例手术中有1至10例患儿死亡。目前,公认的术后并发症危险因素包括:低龄(<3岁)、睡眠呼吸障碍和慢性共病(包括各种神经系统疾病,脑瘫和唐氏综合征)。近日研究人员就美国儿童扁桃体切除术后总体死亡率以及与公认的并发症风险因素的关系进行考察。

本次研究为回顾性队列研究,基于2005-2017年5个州的医疗记录,包括504262名年龄小于21岁的患者数据,患者接受扁桃体切除术伴或不伴腺体切除。研究的主要终点为术后死亡率。
505182 例患儿接受扁桃体切除术,平均年龄7岁,50.6%为女性,其中10.1%为幼儿,28.9%为睡眠呼吸障碍患者,2.8%为复杂慢性疾病患者。共有36例相关术后死亡,平均发生在手术后4.5天,其中大部分(19例,53%)发生在手术出院后。未调整死亡率为7.04例/100 000次手术。多变量模型中,年龄小于3岁和睡眠呼吸障碍与死亡率无显著相关性,但患有复杂慢性疾病儿童的死亡率(16例死亡/14 299例手术)显著高于无共病儿童(20例死亡/490 883例手术,调整后风险比29.39)。患有复杂慢性疾病的儿童占扁桃体切除术患儿的2.8%,但占术后死亡人数的44%。大多数与复杂慢性疾病相关的死亡发生在神经-神经肌肉或先天性遗传疾病的儿童中。
复杂慢性疾病儿童死亡风险较高
研究发现,美国扁桃体切除患儿术后总死亡率为每10万分之7,但对于患有复杂慢性疾病的儿童,其风险高达每10万分之117。
原始出处:
M. Bruce Edmonson et al. Association of Patient Characteristics With Postoperative Mortality in Children Undergoing Tonsillectomy in 5 US States. JAMA,21 June 2022.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#扁桃体切除术#
38
#切除术#
49
#扁桃体切除#
33
#死亡风险#
42
#相关因素#
44
JAMA上文章都是顶级的,谢谢梅斯及时上新
32