Eur Urol:转移去势抵抗性前列腺癌中,激素治疗与化疗获益的预测性基因组生物标志物调查
2021-11-16 AlexYang MedSci原创
新的激素疗法(NHTs),如阿比特龙和恩扎鲁胺,以及基于紫杉类药物的化疗,是治疗转移去势抵抗性前列腺癌(mCRPC)的常用系统疗法。
新的激素疗法(NHTs),如阿比特龙和恩扎鲁胺,以及基于紫杉类药物的化疗,是治疗转移去势抵抗性前列腺癌(mCRPC)的常用系统疗法。预测第二代新型激素疗法(NHT)相对于紫杉类药物益处的生物标志物,对于转移去势抵抗性前列腺癌(mCRPC)患者治疗决策的优化至关重要。对于常见的mCRPC基因组生物标志物,这些关联还未见同时报道。
近期,来自美国的研究人员在《Eur Urol》杂志上发表文章,他们使用已建立的综合基因组分析(CGP)系统,评估了mCRPC常见基因组畸变与治疗获益的关联。
研究为一项回顾性队列设计,使用了来自美国的去身份临床基因组学数据库的数据,该数据库包括了2011年至2020年期间,在常规临床实践中接受治疗的患者,使用了Foundation Medicine CGP对治疗前后获得的组织活检进行了评估。主要队列包括来自308名特定患者的180例NHT和179例Taxane治疗(LOTs)。序列队列为主要队列NHT LOTs的55名患者,且在NHT治疗后直接进行。研究人员评估了患者的前列腺特异性抗原(PSA)反应、两次治疗时间间隔(TTNT)和总生存期(OS)。主要队列分析通过治疗交互模型中的治疗加权的反概率(IPTW),对已知的治疗分配偏差进行了调整。
结果发现,在主要队列中,与没有AR扩增或PTEN畸变的患者相比,有AR扩增(ARamp)或PTEN畸变(PTENalt)的患者对NHT与紫杉类药物的PSA反应更差。有ARamp、PTENalt或RB1畸变(RB1alt)的患者在使用NHT时的TTNT和OS也较差,但使用紫杉类药物时则没有较差。在通过IPTW调整的TTNT和OS的多变量模型分析中,ARamp、PTENalt和RB1alt总体上为不良预后因素,并显示出显著的治疗交互作用,表明了与NHT相比,紫杉类药物的治疗转换和死亡的危险性较低。另外,研究人员仅在连续队列中的ARamp患者中观察到随后的紫杉类药物可使患者获得更多的益处,其中很少有患者有RB1alt用于评估。
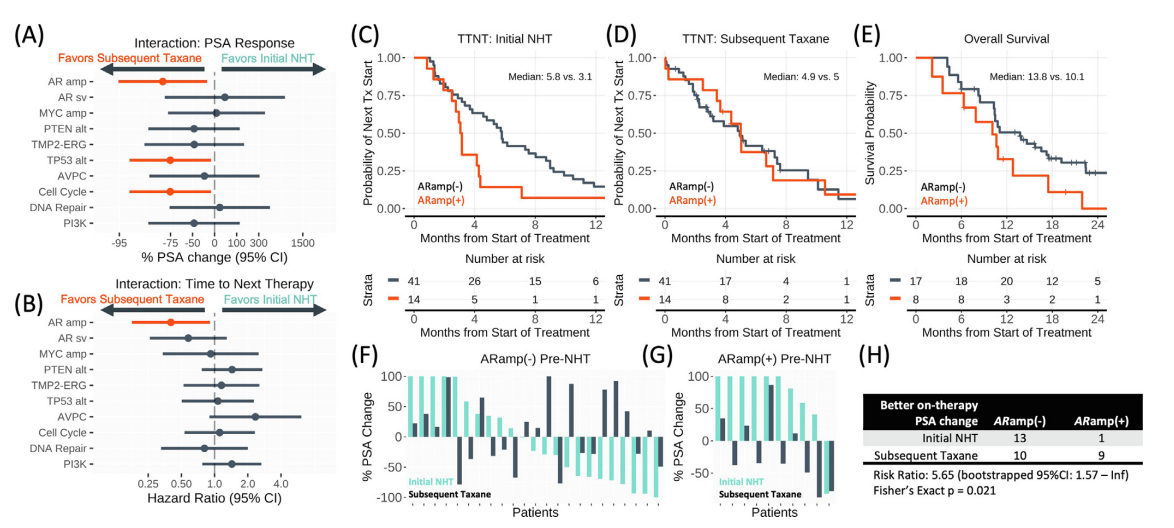
NHT后使用紫杉类药物治疗患者的患者内交叉评估
综上所述,在考虑两种治疗方案的mCRPC疗效时,ARamp状态是预测NHT相对于紫杉类药物效果的一个候选生物标志物。
原始出处:
Ryon P Graf , Virginia Fisher , Joaquin Mateo et al. Predictive Genomic Biomarkers of Hormonal Therapy Versus Chemotherapy Benefit in Metastatic Castration-resistant Prostate Cancer. Eur Urol. Oct 2021
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#抗性#
61
#标志物#
41
#激素治疗#
69
#去势抵抗性前列腺癌#
36
#生物标志#
41
#生物标志#
39