胃粘膜损伤见于多种情况,当损伤因子和防御因子失衡时,就可出现。临床治疗除了祛除病因,选择适当的胃粘膜保护剂对症治疗也很重要。今天就和大家分享一下胃黏膜保护剂及其临床应用特点。
1、铋剂

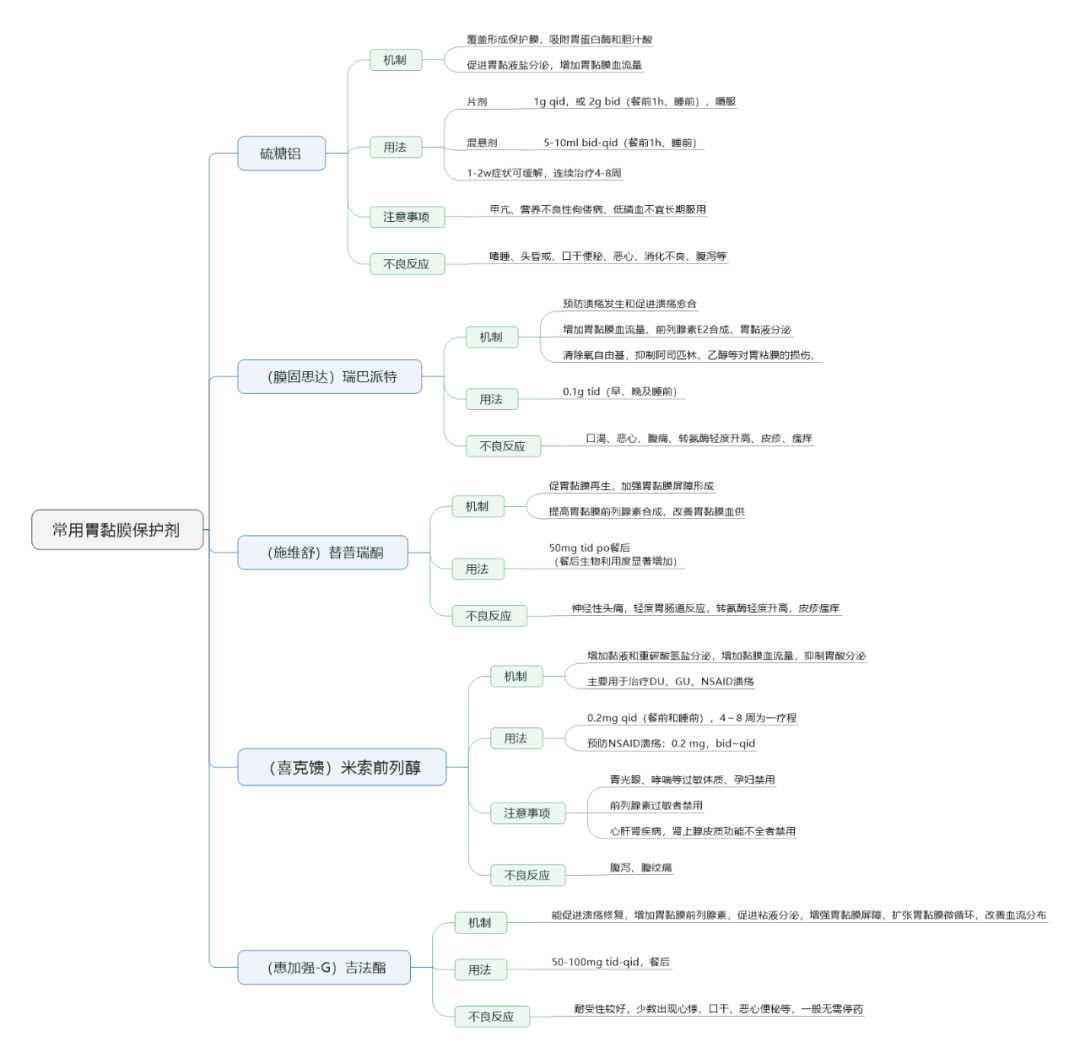
2、常用胃黏膜保护剂
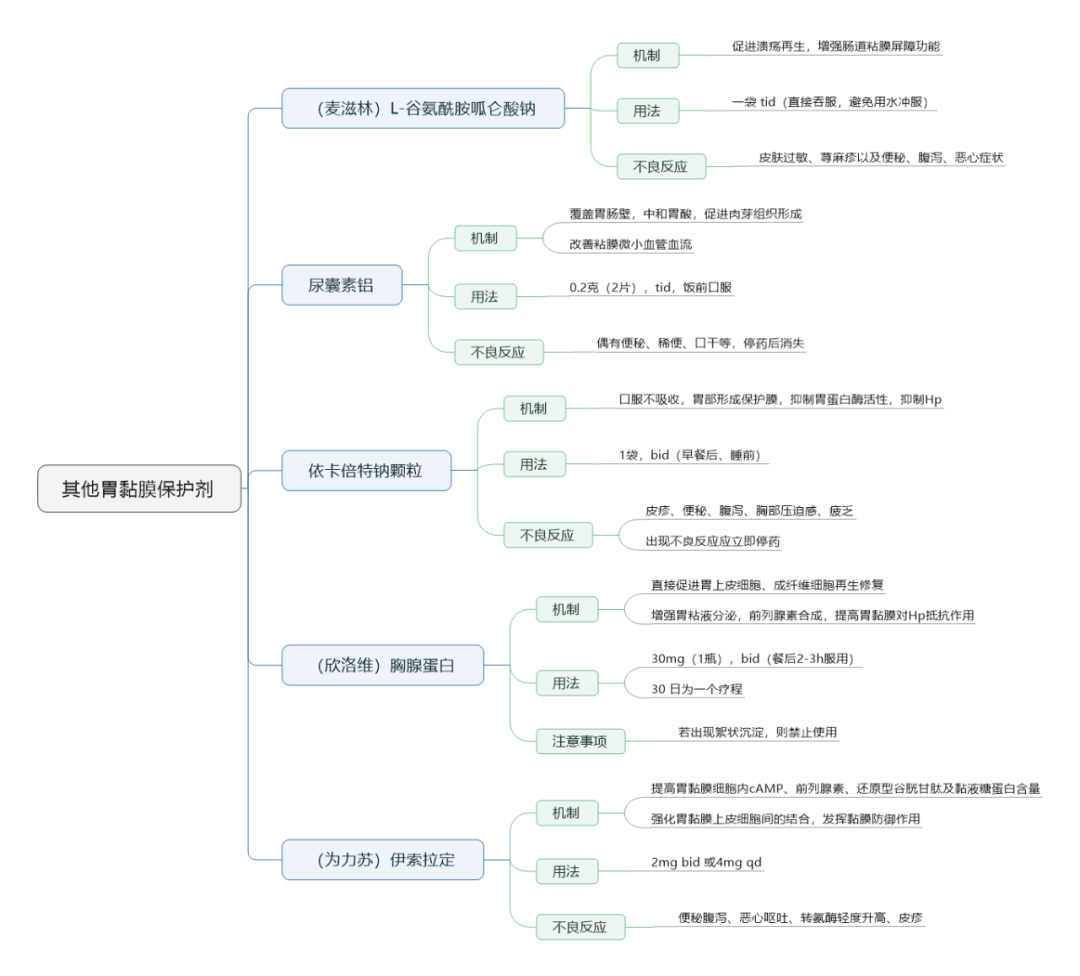
3、其他胃黏膜保护剂
4、胃粘膜保护剂的临床应用
胃粘膜保护剂品种繁多,临床应用过程中,需结合患者特点进行考虑,具体如下:
(1)明确Hp感染者,选用铋剂较为合适,因为其兼具抑制或者杀灭Hp作用。
(2)由胃酸过多引起的胃粘膜损伤,优先使用有抗酸作用或抑制胃蛋白酶活性的药物,比如铝碳酸镁、硫糖铝等,可以发挥抑酸、胃粘膜保护双重药效。
(3)老年人慢性胃炎宜选择如替普瑞酮、铝碳酸镁、瑞巴派特等具有增加黏液分泌、调节黏膜下血流及促进黏膜上皮修复等多重作用的黏膜保护剂。
(4)便秘的患者,不宜使用铝剂、铋剂,因可引起黑便,加重便秘情况;肾功能不全的患者,不宜使用含铝或铋的黏膜保护剂,因肾功能不全,可能会引起体内药物蓄积。
(5)对于酒精或药物引起的胃粘膜损伤,可选择有内源性前列腺素刺激分泌作用药物,如替普瑞酮、瑞巴派特等。
(6)胆汁反流所致的胃黏膜损伤,可选择有吸附胆盐、胆汁酸作用的黏膜保护剂,如铝碳酸镁、硫糖铝和秘剂等。
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#临床应用#
40
#胃黏膜#
49
学习了
48
#黏膜#
48
感谢分享,学习了
45
学习
44