NEJM:脾脏移位-病例报道
2020-11-19 MedSci原创 MedSci原创
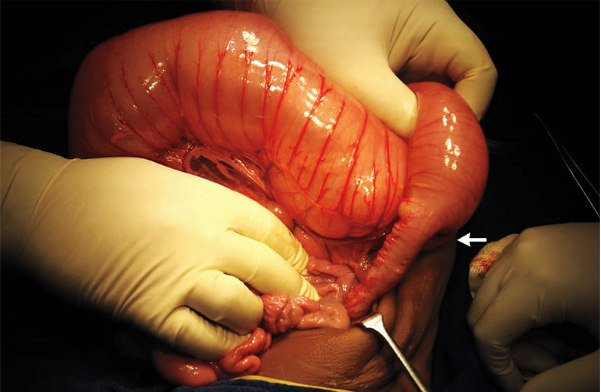
脾脏移位是脾脏韧带松弛导致的罕见病。随着脾脏的移动,可能导致脾门内或脾门附近结构的扭曲,包括胰腺尾巴,这可能会导致急性胰腺炎。对于这种情况的明确治疗是脾切除术。
患者为一名36岁的妇女因腹痛和呕吐1天,而到急诊就诊。她患有溃疡性结肠炎以及因原发性硬化性胆管炎而导致的肝硬化,她的手术史包括全结肠切除术,胆囊切除术和阑尾切除术。
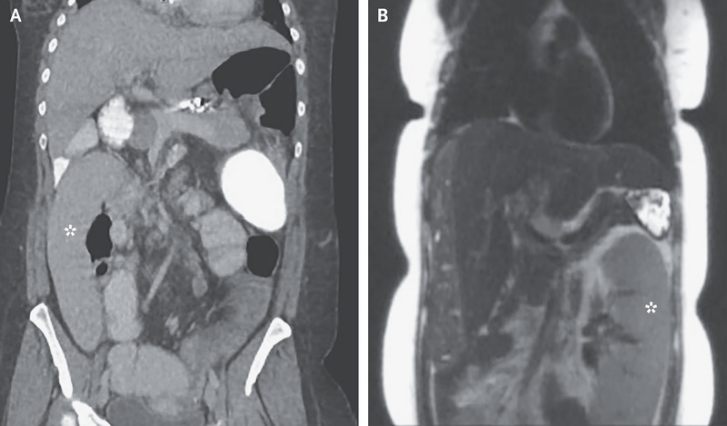
体格检查发现腹部弥漫性压痛。实验室检查发现脂肪酶水平为682 IU/L(参考范围为5至50)。腹部计算机断层扫描发现脾脏位于右下象限(如图A星号所示),胰尾部位于下方和右侧。在本次就诊前两天,患者已通过磁共振胆胰胰管造影术进行了肝细胞癌的常规筛查,该检查显示脾脏位于腹部左侧(如图B星号所示),以及胰腺正常,未见胆结石。
脾脏移位是脾脏韧带松弛导致的罕见病。随着脾脏的移动,可能导致脾门内或脾门附近结构的扭曲,包括胰腺尾巴,这可能会导致急性胰腺炎。对于这种情况的明确治疗是脾切除术。
该患者接受了肠胃外疼痛控制治疗和补液治疗,腹痛和呕吐得以缓解。由于该患者正在进行肝移植评估,因此推迟了脾切除术。
原始出处:
Alexander Wester,et al.Wandering Spleen.N Engl J Med.2020;https://www.nejm.org/doi/full/10.1056/NEJMicm2003627
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










好文章!
108
学习病例
110
非常好的病例
107
学习了
109
顶刊就是顶刊,谢谢梅斯带来这么高水平的研究报道,我们科里同事经常看梅斯,分享梅斯上的信息
72
好的
76
学习中
36
谢谢
51
666
43
学习中
30