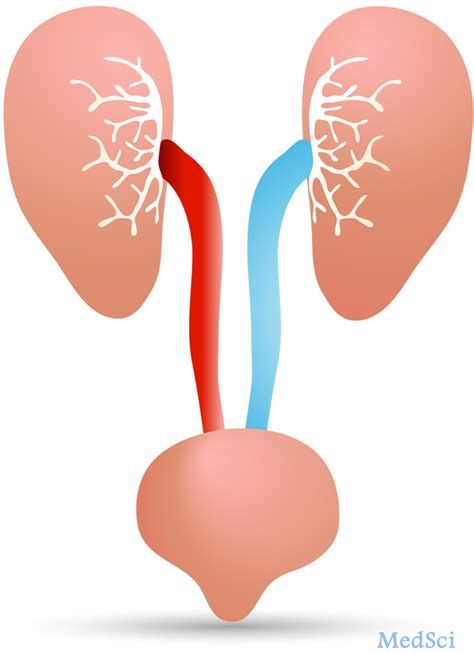
Oncol Lett:miR-26a-5p表达增强能够通过靶向PTEN促进膀胱癌的发展
2018-10-03 AlexYang MedSci原创
最近,有研究人员评估了miR-26a-5p在膀胱癌(BC)发展过程中的表达和特异性角色。研究人员利用RT-PCR技术评估了miR-26a-5p在BC中和健康对照中的表达水平。研究发现,miR-26a-5p的表达在BC患者中显著增加。进一步的是,BC组织与临近的非瘤组织-26a-5p相比,miR-26a-5p表现出了更高的表达水平。在Ta-T1阶段,与BC患者喜爱那个比,miR-26a-5p的表达水
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#Oncol#
48
#miR#
52
这只不过是在数据库里串的一个小通路而已
100
#PTEN#
52
谢谢分享,学习了
82
学习了谢谢分享
59
感谢小编为我们准备了如此丰盛的精神大餐,同时也向作者致谢!认真学习了,点赞!
57