FDA不建议COVID-19患者使用非甾体抗炎药(NSAID)
2020-03-20 Allan MedSci原创
FDA报道指出,使用非甾体抗炎药(NSAID)(如布洛芬)可能会使新型冠状病毒(COVID-19)肺炎恶化。
FDA报道指出,使用非甾体抗炎药(NSAID)(如布洛芬)可能会使新型冠状病毒(COVID-19)肺炎恶化。在2020年3月11日发表于《柳叶刀》的一项研究指出,NSAID可能加剧COVID-19肺炎患者的症状。
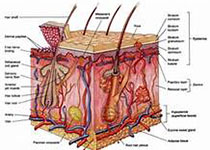
目前,FDA还不清楚将布洛芬等NSAID与COVID-19症状的恶化联系起来的科学证据。该机构正在进一步调查此问题,并将公布更多信息。对于那些希望使用NSAID以外的治疗选择的人,有多种非处方药(OTC)和处方药被批准用于缓解疼痛和减少发烧。
FDA建议公众在使用NSAID前应阅读完整的《药物概况》标签。当公众遵循标签上的指示和/或健康护理专业人员的指示时,OTC药物是安全有效的。使用处方药的患者应按照医疗保健专业人员的指示并按照标签上的说明服用这些药物。
原始出处:
https://www.firstwordpharma.com/node/1709518
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#AID#
42
#不建议#
54
#SAID#
50
#COVID-19患者#
43
#非甾体抗炎药#
54
#抗炎药#
47
#NSAID#
27