Oral Dis:龋齿与肝移植有关吗?一项系统回顾和荟萃分析
2021-10-28 MedSci原创 MedSci原创
在肝衰竭的病人进行肝脏移植治疗期间,口腔卫生困难以及唾液和口腔微生物菌群的变化可能会增加牙齿生物膜的致病潜力。
龋齿是一个动态过程的结果,其特点是牙齿结构的脱矿期和再矿化期,是由于不正常的生物膜对糖的代谢造成的。
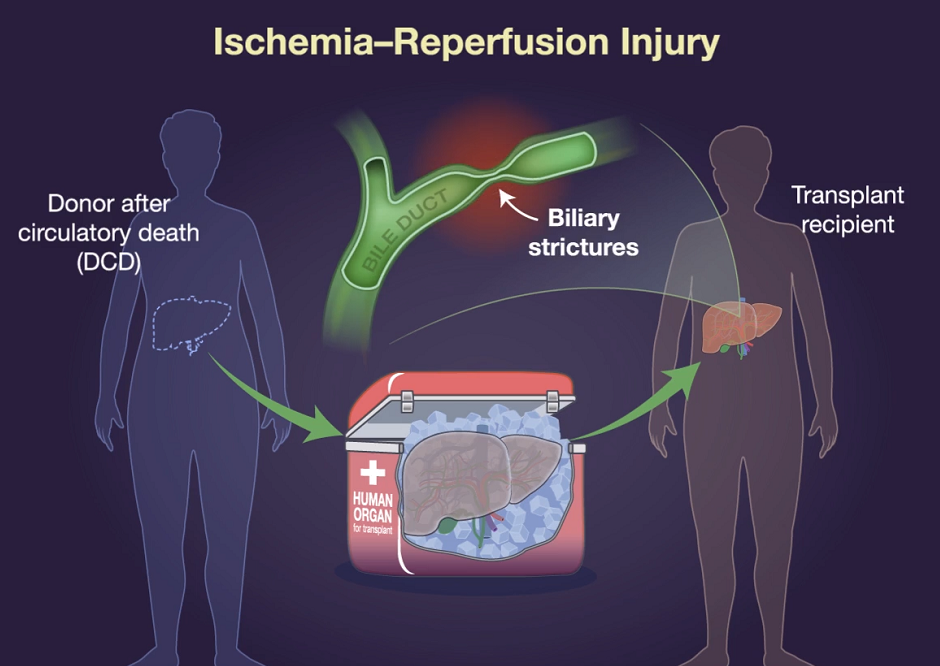
对于病毒性肝炎(B和C)、原发性胆汁性肝硬化以及药物引起的肝损伤等所导致的不可逆转的肝衰竭患者,肝移植是其指征性疗法。由于移植后存在移植排斥的风险,患者要接受免疫抑制药物的治疗,药物的长期使用会降低个人的免疫能力。在移植治疗期间,口腔卫生困难以及唾液和口腔微生物菌群的变化可能会增加牙齿生物膜的致病潜力。此外,患有原发性胆汁性肝硬化和慢性肝炎的人可能会出现唾液分泌减少,以及随之而来的唾液蛋白和酸缓冲能力的降低,可能会增加龋齿的风险。
尽管文献中报道了接受肝移植的个体有较高的龋齿发病率,但这种关联尚未完全阐明。为了评估这个问题的现有科学证据,发表于Oral Dis的一项系统综述和荟萃分析评估了肝移植前或肝移植后个体的龋齿经历
研究人员检索了PubMed、Scopus、Web of Science、Ovid和Lilacs等数据库,检索时间从数据库的开始日期到2020年4月为止。此外,研究人员还进行了灰色文献和人工搜索。检索到的参考文献由两名独立审查员进行评估。使用阿德莱德大学的工具进行了元分析和偏倚风险评估。使用GRADE评估证据的强度。
结果,研究人员共检索到了1990份参考文献,最终纳入了24项横断面研究。一项亚组分析显示,肝移植前的人和健康的人在患龋齿的牙齿数量上没有显著差异(平均差异=1.65,置信区间=-0.87至4.17)。肝移植前个体的龋齿发生率为73.82%,移植后个体的龋齿发生率为72.83%。在纳入的研究中,关于偏倚风险的主要关注点是缺乏对混杂变量的控制。证据的强度非常低。

综上所述,该研究结果表明,龋齿可能是肝移植前后个体的一个相关问题。口腔健康咨询应包括在对肝移植前和/或肝移植后个体的护理中。
原始出处:
Carla de Souza Oliveira, et al., Is dental caries associated with liver transplantation? A systematic review and meta-analysis. Oral Dis. 2021 Sep;27(6):1346-1355. doi: 10.1111/odi.13439. Epub 2020 Jun 25.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#荟萃#
38
#荟萃分析#
45
#Oral#
46
#Dis#
41
#系统回顾#
44
学习了,谢谢分享
61