European Radiology:盆腔MRI显示的腹膜转移在直肠癌患者的分期中有何价值?
2022-08-05 shaosai MedSci原创
直肠癌文献中有丰富的放射学和病理学的相关研究支持MRI在显示肿瘤累及直肠系膜脂肪和筋膜及周围器官的程度方面的准确性和预测价
前腹膜即解剖学上离直肠最近的内脏腹膜(VP),可在大多数专门的直肠磁共振成像(MRI)检查中很好地勾勒出来。然而,直肠癌的腹膜转移(PC)的影像学或临床病理诊断并不常见。
随着研究的深入,人们认识到结肠癌和直肠癌的VP侵犯这一类别的患者比肿瘤侵犯其他邻近结构和器官(T4b)的患者有更好的5年生存率,因此在美国癌症联合委员会第七版指南中将这类患者分为一个独立的T4疾病类别(T4a)。直肠癌文献中有丰富的放射学和病理学的相关研究支持MRI在显示肿瘤累及直肠系膜脂肪和筋膜及周围器官的程度方面的准确性和预测价。然而,关于基于MRI的VP侵袭及其与PC的关系或其预示临床结果的能力的研究十分很缺乏。
近日,发表在European Radiology杂志的一项研究将直肠癌中基于MRI的VP侵犯与基线MRI时存在的PC以及临床随访期间PC的发展联系起来,探讨了cT4a与PC的实际关联,为临床进一步精确直肠癌患者的风险分层及预后预测提供了参考依据及技术支持。
本研究从,由两位放射科医生回顾了2013年-2018年临床(c)T3c、cT3d、cT4a和cT4b的原发性直肠腺癌患者的治疗前直肠MRI图像的临床病理记录,并记录了标准的MRI描述和病理分期。使用Kaplan-Meier方法估计无复发(RFS)和总生存(OS)。使用竞争风险分析探讨了PC的发展,存活率的差异用对数rank检验进行比较,并使用Gray's检验来检验PC的CUIN差异。
共纳入343名患者(147名女性;中位年龄56岁)的MRI分期为cT3cd,n = 170;cT4a,n = 40;和cT4b,n = 133。幸存者的中位随访时间为27个月(0.36-70个月)。对于M1患者,OS仅因cT分期而不同(2年OS:cT3 88.1%,cT4a 79.1%,cT4b 64.7%,p = 0.045)。对于M0患者,OS和RFS仅因病理(p)T分期而不同。本研究观察到PC的累积发生率按cT分期有统计学上的显著差异(2年CUIN:cT3 3.2%,cT4a 8.5%,cT4b 1.6%,p = 0.01),但按pT分期没有差异。79名患者(23%)出现了转移性病灶(M1),8名患者有PC(2.3%)。总体而言,8名患者出现了PC(cT4a:n = 4,其他阶段:n = 4),22名患者发展为PC(cT4a:n = 5,其他阶段:n = 17)。
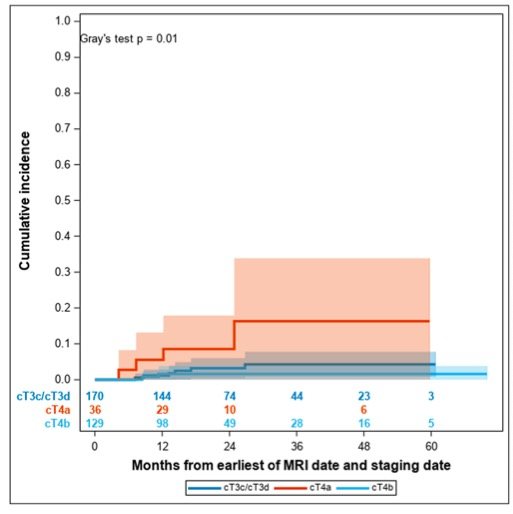
图 按临床T分期划分的腹膜转移病灶的发生时间
在本研究的直肠癌临床晚期患者中,PC并不常见,但PC的发生时间与基于MRI的T分期有关,并且在诊断为cT4a的患者中发病率更高。鉴于PC的临床重要性及其在肿瘤学上的挑战,本研究认为有必要进一步研究患者的基因组学和特定的影像学高危征象以更好地进行患者护理及评估。
原文出处:
Marc J Gollub,Stephanie Lobaugh,Jennifer S Golia Pernicka,et al.Occurrence of peritoneal carcinomatosis in patients with rectal cancer undergoing staging pelvic MRI: clinical observations.DOI:10.1007/s00330-022-08694-7.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#PE#
40
😃
34
#腹膜转移#
43
#腹膜#
36