宋光远:知难而进——CTO开通策略中球囊的应用
2021-01-31 《门诊》杂志 门诊新视野
在开通CTO术中,无论前向或逆向技术,都会应用到球囊。目前冠脉分叉病变的介入治疗中,必要性支架技术使用比例较高,而球囊保护技术在操作过程中能保证边支血管的持续开通。
在开通CTO术中,无论前向或逆向技术,都会应用到球囊。目前冠脉分叉病变的介入治疗中,必要性支架技术使用比例较高,而球囊保护技术在操作过程中能保证边支血管的持续开通,但相对于导丝保护技术,分支血管的球囊保护技术操作比较复杂。一般而言,对于血管较大、分支的支配范围较大、分叉成角较小的病变部位,预测单纯导丝保护情况下主支支架植入后边支闭塞风险高的情况,建议采用球囊保护技术。球囊边支保护技术是一种预防措施,在主支释放支架后出现边支闭塞情况时,术者可以从容处理开通闭塞,保证边支血液供应。
CTO解剖病变对开通策略的影响
CTO开通的术前决策至关重要,而CTO病变的解剖特点对开通策略的选择影响重大,主要包括病变的性质、长度、成角情况,闭塞段两侧入口情况以及闭塞段周围分支情况等三个方面(图1)。正因如此,每位患者在术前应进行冠状动脉CT检查以帮助术者制定开通CTO策略。
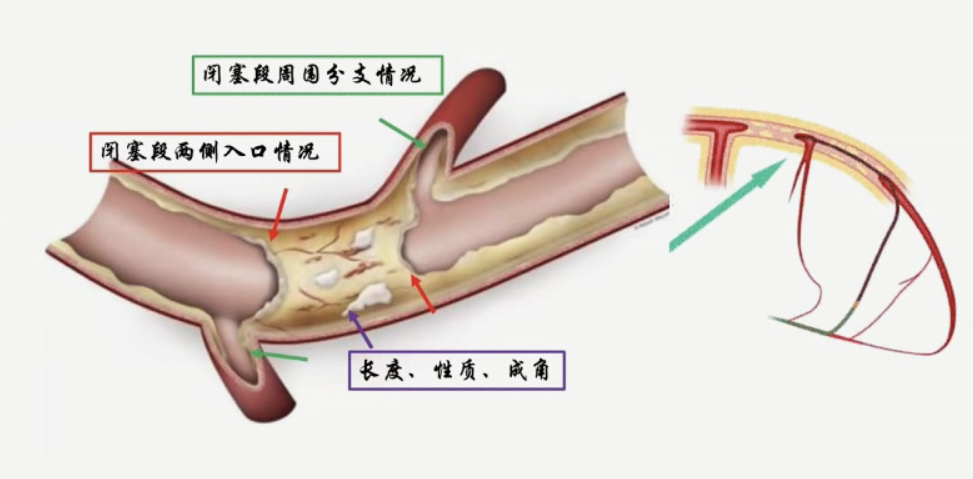
图1. 影响CTO开通策略的解剖结构
无论选择前向或逆向技术,抑或是内膜下再进入技术,都会应用到球囊保护技术(图2),其在操作过程中能保证边支血管的持续开通。一般而言,对于血管较大,分支的支配范围较大,分叉成角较小的病变部位,预测单纯导丝保护情况下主支支架植入后边支闭塞风险高的情况,建议采用球囊保护技术。术中我们通常要准确选择球囊的尺寸、锚定位置等以保证后续手术的顺利完成。

图2. CTO开通策略中球囊的应用
CTO开通策略中球囊的应用
球囊锚定
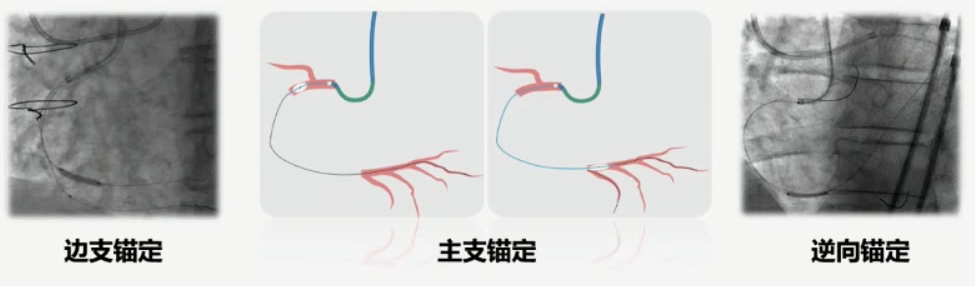
对于进行开通CTO的术者而言,球囊锚定是采取的常规策略。在右冠CTO开通中,Guiding到位后往往支撑较差,此时往往通过边支球囊锁定增强指引导管的支撑力。而在选择球囊时我们首先应关注锚定的部位(边支锚定、主支锚定、逆向锚定),过程如下:
工作导丝进入边支(右冠通常为a conus oracute marginal branch,左冠前降支通常为a diagonal);
跟进小尺寸球囊(直径选择参考边支血管直径,通常为1.5~2.0 mm);
球囊以6~8 atm压力扩张,锚定指引导管同时增加后续器械如球囊及微导管的输送能力,此时需注意在边支球囊扩张时,可能引发患者胸痛。
正向内膜下重回真腔技术(STAR)
STAR技术是指当导丝进入假腔后,尝试在假腔远端再次进入血管真腔,常将导丝头端在假腔中成袢,利用Knuckle技术,即将内膜下Knuckle的导丝(一般多为聚合物护套导丝如Pilot)强力前推,在某一分支前形成钝性分离,直至远端撕裂回真腔,球囊跟进后,在内膜下进行球囊扩张术,操控导丝再进真腔,示例如图(图3)。MINI-STAR技术则是指在CTO病变附近制造小的夹层,然后用硬导丝通过病变到达远端血管真腔。Contrast-guided STAR技术指从微导管内,以较高压力注射造影剂,使得CTO病变近端产生夹层,从而使导丝通过病变,重新进入真腔,因此又称为造影剂引导的STAR技术,相比较传统STAR技术,操作相对温和。
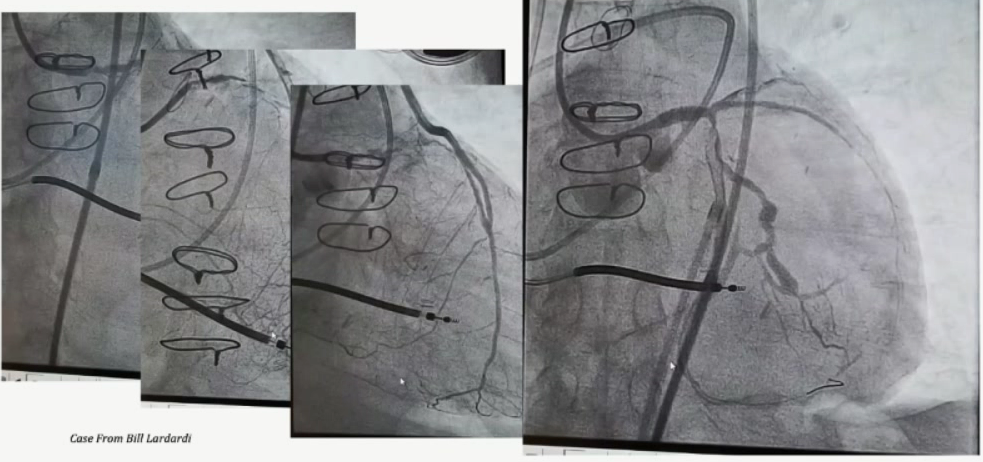
图3.正向内膜下重回真腔技术示例
控制性正向-逆向内膜下寻径技术(CART)
CART技术的基础是通过逆向导丝送入球囊进行扩张,在CTO段制造一个有限撕裂的内膜下夹层,加强辅助前向导丝的通过(图4),但该技术操作复杂,夹层不可控,风险较大,目前临床应用较少。操作要点如下:
逆向导丝通过间隔支侧支后,通过微导管或小尺寸球囊扩张(不建议用球囊扩张心外膜侧支);
选择合适尺寸的球囊沿逆向导丝进入闭塞病变段,与前向器械向交汇;
低压力扩张撕裂内膜扩大假腔,通过球囊制造的空间打通正向与逆向的通路;
再次调节前向导丝传入逆向球囊撕裂的假腔,同时调节导丝以逆向导丝为参照,推送导丝进入远端真腔。
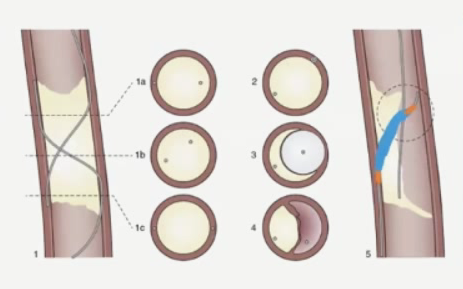
图4. 控制性正向-逆向内膜下寻径技术
反向控制性正向-逆向内膜下寻径技术(R-CART)
反向CART是逆向介入治疗中最为重要的一种技术,临床中颇为常用。该技术的基础是通过前向导丝送入球囊进行扩张,在CTO段制造一个内膜下的夹层,通过这个假腔空间辅助逆向导丝的通过。具备操作相对简便,可重复性高的优势。操作要点如下:
当逆向与前向导丝均走行于内膜下时应尽量让两根导丝相互靠近,并通过多体位投照证实两者确有相互交汇;
经正向导丝送入球囊扩张闭塞病变,造成一个假腔。正向扩张球囊的直径尺寸应根据正逆向导丝之间的距离预估,通常选用2.0~4.0 mm直径的球囊;
正向球囊扩张的同时,操作逆向导丝沿球囊方向行进;在正向球囊解压时操作逆向导丝沿球囊方向行进。此时即使逆向导丝进入了假腔,正向球囊的扩张力也可减小假腔范围与大小。
前向内膜下再进入技术(ADR)
如果术者无法将导丝从近端真腔送入远端真腔,可以考虑选择ADR技术,使导丝进入前向内膜下再进真腔。ADR技术的步骤分为3步:近端纤维帽的突破,球囊快速到达远端着陆区,导丝重入真腔。重入真腔有“4S”原则:
Stabilize:稳定,指球囊不能在血肿里飘,位置牢固才能有效穿刺;
Straw:当血肿较大时可抽吸血肿;
Stick:有效的穿刺;
Swap:当导丝扎入远端真腔后,顺着该孔道换入工作导丝有利于后续操作。
宋光远教授主要介绍了基于Stingray球囊的ADR技术,该技术适合闭塞段>20 mm的长段闭塞病变,并可应对近端纤维帽模糊,无残端的病变,以及闭塞远端血管有落脚点及纤维帽处无分支,逆向(侧支)条件差的情况;当Stingray球囊无法通过CTO阶段时,可尝试1.2~1.5 mm小球囊扩张。此外,血肿的控制是ADR技术成功的关键点之一。如果血肿较大,可以在导丝穿刺以前抽吸血肿;另外,指引导管到位后即送入Guidezilla导管靠近CTO节段也是控制血肿的好办法。需注意的是Guidezilla+Stingray的方法需快速和高效,时间越长,发生血栓的几率就越高。
CTO开通中球囊的选择
CTO病变介入治疗中,球囊的合理选择能够有效提高CTO-PCI的手术成功率。选择预处理球囊时应遵循的基本原则如下:
选择通过性好的球囊:一般选用表面具有超滑涂层、通过外径小的单嵌入式标记球囊,通过钙化病变时宜选球囊头端短而硬的球囊,通过迂曲病变时优选球囊头端细小而圆润的球囊;
选择推送力强的球囊:推送力强传递更为高效;
选择灵活性和跟踪性更好的球囊。
随着ADR技术的发展,相关器械亦不断更新迭代,作为进口球囊之一,MINI TREK球囊在开通CTO成功率方面表现出众,其光滑圆润的头端设计具有不容易被钙化的特点,在提高通过性的同时提升了头端的耐用性,此外还减少了对血管和支架结构的损伤。EXPERT CTO研究旨在探索MINI TREK球囊在CTO开通中的应用,在88个CTO病变中使用了125个MINI TREK球囊,研究首要终点为即刻通过性及病变扩张成功率。即刻手术成功率达100%(器械成功通过,治疗后病变残余狭窄<50%);围手术期未发生死亡和靶病变再次血运重建,MACE事件发生率为2.27%(2/88),心梗发生率为1.4%。结果提示,MINI TREK在CTO病变预处理中具有即刻成功率高的优异表现,并有助于提高临床CTO-PCI的安全性和手术效率。
总 结
宋光远教授最后总结道,CTO作为PCI最后难以攻下的“堡垒”,其临床病例复杂多变,实际治疗往往存在各种困难。然而随着技术的进步,多学科协作模式的建立,为广大介入医师提供了更好的操作平台;介入医师应积极学习新技术并立足于扎实的基础理论,做好充足准备的同时做到勇气与踏实并存,不断地去尝试攻克CTO开通中的难关。而球囊的选择与应用是开通CTO的重要环节,精准操作球囊可大幅提高CTO的开通效率,因此每一位进行CTO开通的术者均需娴熟掌握CTO球囊的规范及技巧,将之灵活应用于临床,为患者带来更好的手术效果。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#CTO#
54
学习了
86
#球囊#
0
感谢
93
棒
95
棒
79