透明隔区毛细胞型星形细胞瘤1例
2020-02-10 刘闯 孙召龙 马红玉 医学影像学杂志
患者女,50岁。间断性头晕行头颅CT、MRI平扫+强化检查,显示侧脑室室间孔无强化肿块,考虑胶质瘤。入院CT检查:双侧侧脑室之间占位性病变,密度混杂,多发钙化影,边界不清,最大截面积约2.1 cm×2.8 cm(图1A)。MRI平扫:透明隔处肿块,大小约3.2 cm×3.0 cm×1.9 cm,信号不均匀(图1B),增强扫描时肿物未见异常强化(图1C)。实验室检查:血糖15.45mmol/L,糖化
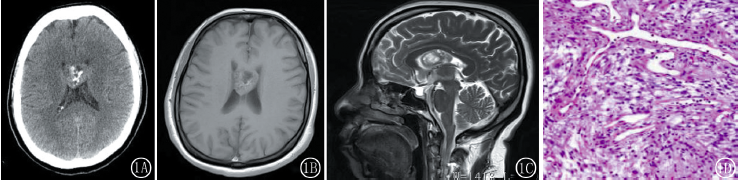
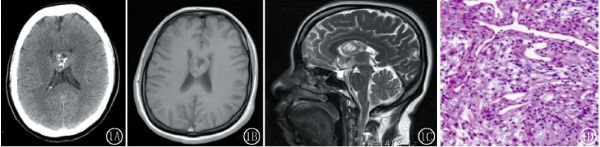
患者女,50岁。间断性头晕行头颅CT、MRI平扫+强化检查,显示侧脑室室间孔无强化肿块,考虑胶质瘤。入院CT检查:双侧侧脑室之间占位性病变,密度混杂,多发钙化影,边界不清,最大截面积约2.1 cm×2.8 cm(图1A)。MRI平扫:透明隔处肿块,大小约3.2 cm×3.0 cm×1.9 cm,信号不均匀(图1B),增强扫描时肿物未见异常强化(图1C)。实验室检查:血糖15.45mmol/L,糖化血红蛋白4.01mmol/L,尿蛋白(+-)、葡萄糖4+。糖尿病科会诊:2型糖尿病。全麻下行开颅颅内肿瘤切除术,术后经天津市环湖医院病理诊断:毛细胞性星形细胞瘤(WHOI级)(图1D)。
图1A透明隔区团状软组织影,密度不均匀,可见囊变及钙化影,边界清楚,周围无水肿;图1BT1WI病变呈等、低混杂信号;图1C矢状位T2WI病变呈等、高混杂信号;图1D病理图片,肿瘤细胞呈梭形,排列呈束装,可见大量嗜酸性小体(×200,HE)
讨论
毛细胞型星形细胞瘤2016年WHO中枢神经肿瘤分级定位I级,发病率低,好发于10~20岁的儿童及青少年。肿瘤病理学特征为细长排列较疏松的瘤细胞,双极纤维细胞常分布在血管周围,可见较明显增生的血管,瘤内可见数量不等的Rosenthal纤维。肿瘤实质内可出现假栅栏样坏死和凋亡现象,提示肿瘤实质内的小囊肿。
肿瘤沿蛛网膜下腔或软脑膜侵犯周围脑组织,这与其生长缓慢、良性的生理性行为相矛盾。毛细胞型星形细胞瘤CT多为境界清楚的低密度,内部可见大小不等的囊变,肿瘤周围可见钙化,肿瘤周围多无脑水肿为其典型特征之一,发生于小脑半球典型的毛细胞星形细胞瘤为囊性伴实性壁结节,增强扫描实性部分会出现较明显的强化,MRI与CT表现相似,实性部分呈长T1稍长T2信号影,有囊变的部分往往T1WI信号更低,T2WI信号更高,肿瘤出血少见,水肿程度低,更容易发现肿瘤侵袭蛛网膜下腔和软脑膜的情况。
本例患者MRI信号混杂,实质呈稍长T1稍长T2影,病变内可见明显囊变。中线处第三脑室旁的毛细胞星形细胞瘤需要与中枢神经细胞瘤、节细胞胶质瘤相鉴别。中枢神经细胞瘤发病率很低,可见条形及环状钙化,肿瘤常呈多囊样改变,表现为“蜂窝状”或“丝瓜瓤”样改变,DWI成像肿瘤呈高信号,肿瘤由于血供丰富,常常有流空血管影。节细胞胶质瘤发病年龄为5岁之前和40岁左右,肿瘤大部分呈实性或囊实性,囊伴结节为肿瘤特征性表现,强化扫描可见多发散在结节样明显强化影。影像学检查价值在于术前明确诊断和指导手术方案,以便临床术后观察及评价预后。
原始出处:
刘闯,孙召龙,马红玉.透明隔区毛细胞型星形细胞瘤1例[J].医学影像学杂志,2019,29(01):32+123.
小提示:本篇资讯需要登录阅读,点击跳转登录
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#透明隔区#
26
#毛细胞型#
40
#细胞瘤#
19