Lancet Rheumatology: 原发性系统性血管炎或风湿性多肌痛患者COVID-19的结果:一项回顾性队列研究
2021-11-19 MedSci原创 MedSci原创
在原发性系统性血管炎和风湿性多肌痛患者中,严重的COVID-19结局与年龄、性别、合并症数量以及治疗方法(包括大剂量糖皮质激素)等多个风险因素相关。
背景:由于所使用的治疗方法、原发性系统性血管炎引起的潜在器官损伤以及与这些疾病相关的人口统计学因素,原发性全身性血管炎或风湿性多肌痛患者可能面临COVID-19不良结局的高风险。因此,研究者旨在调查与原发性系统性血管炎或风湿性多肌痛患者COVID-19结局相关的因素。
方法:在这项回顾性队列研究中,2020年3月12日至2021年4月12日期间被诊断为COVID-19、有原发性系统性血管炎(抗中性粒细胞胞浆抗体 [ANCA] 相关血管炎、巨细胞动脉炎、白塞氏综合征或其他血管炎)或风湿性多肌痛病史的患者,报告给COVID-19全球风湿病联盟登记处。为了评估患者的COVID-19结果,研究者使用了等级COVID-19严重程度量表,定义为:(1)未住院;(2)住院未吸氧;(3) 住院期间有任何补充氧气或通气;或 (4) 死亡。多变量有序逻辑回归分析用于估计比值比(OR),调整年龄、性别、时间段、合并症数量、吸烟状况、肥胖、糖皮质激素使用、疾病活动、地区和药物类别。分析也按风湿性疾病的类型进行了分层。
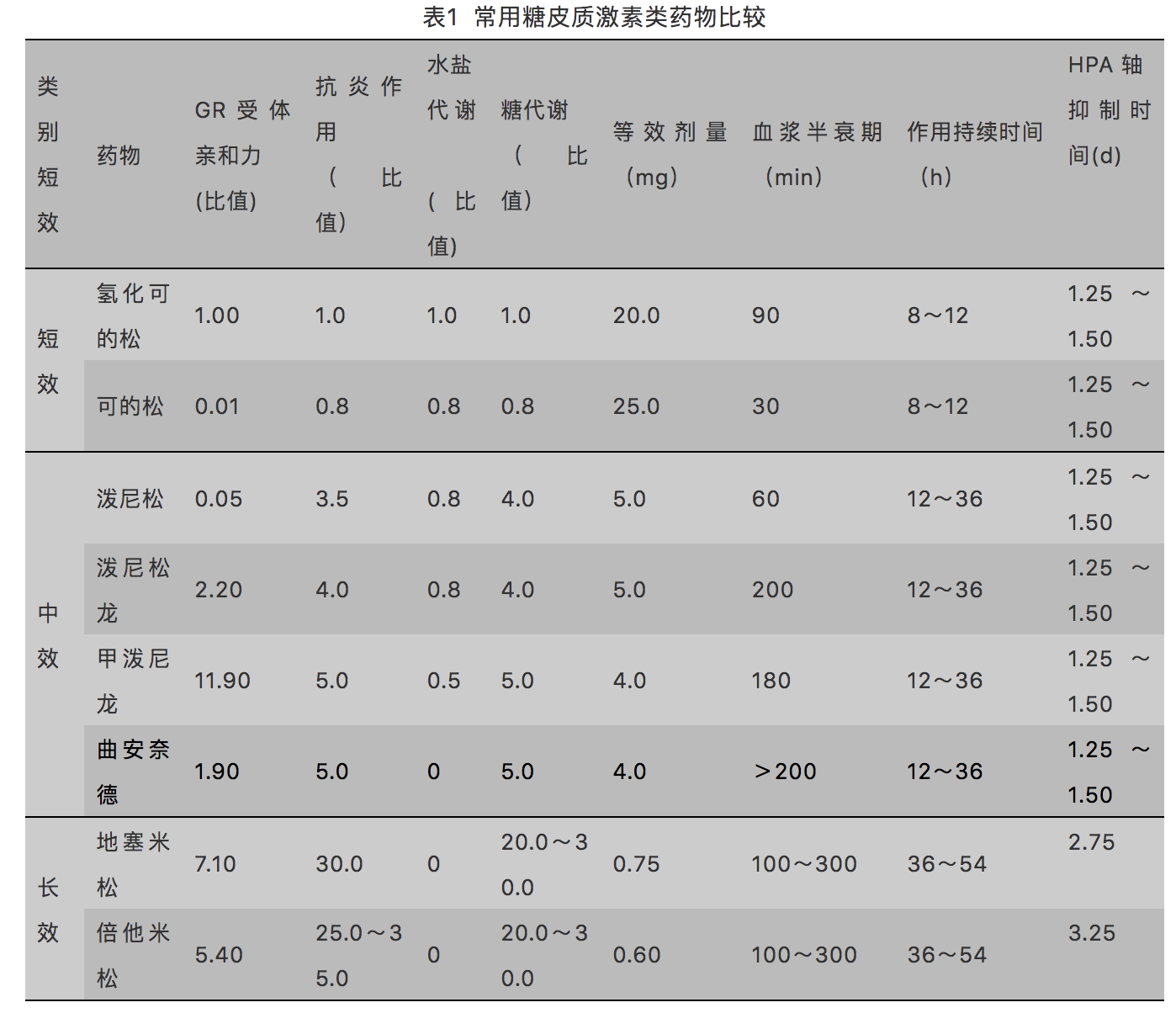
结果:在注册登记的1202名符合条件的患者中,733名(61.0%)为女性,469名(39.0%)为男性,平均年龄为63.8岁(SD 17.1)。共有374 (31.1%)名患者患有风湿性多肌痛,353名 (29.4%)名患有ANCA相关性血管炎,183名(15.2%) 名患有巨细胞动脉炎,112名(9.3%)患有Behçet综合征, 180 (15.0%) 有其他血管炎。在有结果数据的1020名(84.9%) 患者中,512名(50.2%) 未住院,114名(11.2%)住院且未接受补充氧气,239名(23.4%)住院且接受通气或补充氧气,155人(15.2%)死亡。在以下情况观察到COVID-19结局不佳的几率更高:年龄较大(每增加10岁的OR 1.44 [95% CI 1.31–1.57]),男性(与女性相比的OR 1.38 [1.05-1.80]),有更多的合并症(每增加一个并发症OR为1.39 [1.23-1.58]),服用10 mg/d或更多的泼尼松龙(与不服用相比OR为2.14 [1.50-3.04]),或与疾病缓解或疾病活动度低的患者相比具有中度、高度或重度疾病活动度 (2.12 [1.49-3.02])。不同疾病亚型的危险因素不同。
小结:在原发性系统性血管炎和风湿性多肌痛患者中,严重的COVID-19结局与年龄、性别、合并症数量以及治疗方法(包括大剂量糖皮质激素)等多个在很大程度上不可改变的风险因素相关。该研究结果可用于为患有这些疾病的患者提供缓解策略。
出处:
Sattui, Sebastian EDahou, Brahim et al. Outcomes of COVID-19 in patients with primary systemic vasculitis or polymyalgia rheumatica from the COVID-19 Global Rheumatology Alliance physician registry: a retrospective cohort study. The Lancet Rheumatology, Volume 0, Issue 0
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#系统性#
43
#Lancet#
46
#Rheumatology#
39
#原发性#
45
#血管炎#
49