Nature Cancer:仁济医院高维强教授发现Gremlin1可能是去势抵抗性前列腺癌治疗新靶点
2022-06-02 上海交通大学医学院附属仁济医院 上海交通大学医学院附属仁济医院 发表于威斯康星
本文为靶向治疗去势抵抗性前列腺癌提供了新型候选药物,具有重要的临床转化意义。
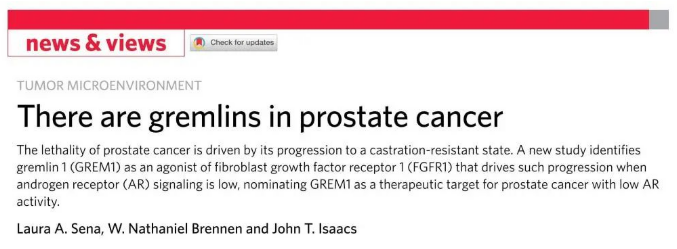
近日,上海交通大学医学院附属仁济医院、癌基因及相关基因国家重点实验室、上海市肿瘤研究所朱鹤研究员和高维强教授等在肿瘤权威期刊《Nature Cancer》(即时影响因子为23)上发表了分泌蛋白Gremlin1治疗去势抵抗性前列腺癌(CRPC)的科研成果,揭示了Gremlin1作为FGFR1新型配体,通过FGFR1/MAPK信号通路调控肿瘤细胞可塑性、促进CRPC发生发展以及Gremlin1特异性抗体的应用治疗研究。前列腺发育和前列腺癌研究的国际知名专家John Isaacs还为本文在《Nature Cancer》杂志撰写了重点介绍。
雄激素受体信号通路(androgen receptor pathway)是前列腺癌(prostate cancer,简称PCA)发生发展中的关键因素。靶向拮抗AR信号通路的雄激素剥夺疗法(androgen deprivation therapy, 简称ADT)是临床上最为经典的治疗手段之一,然而多数患者在短期疾病缓解后会出现治疗抵抗并且复发成去势抵抗性前列腺癌(castration-resistance prostate cancer, 简称CRPC)。CRPC预后差,致死率高,是一种复杂的异质性肿瘤。
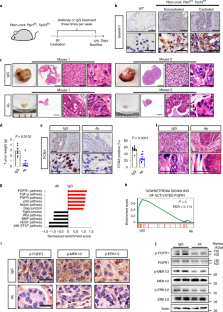
Gremlin1是一种高保守型分泌蛋白,通过与BMP-2,BMP-4以及BMP-7特异性结合的方式,抑制BMP配体与相应受体结合,参与调控胚胎时期骨组织、肾脏等重要器官发育。研究人员发现,Gremlin1通过拮抗BMP信号通路参与了多种肿瘤的恶性进展,比如脑胶质瘤、结直肠癌、肺癌等。在本文中,作者证实Gremlin1在去势抵抗性前列腺癌中特异性的高表达,而该蛋白的转录表达受到AR的直接反向调控。只有当机体内含有较高浓度的雄激素时,AR才能有效抑制GREM1表达分泌,这也就导致Gremlin1蛋白在机体接受ADT治疗后表达水平会显著增加。Gremlin1可以在体内外有效促进前列腺癌在雄激素剥夺的环境中发生发展。



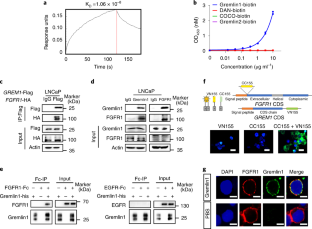
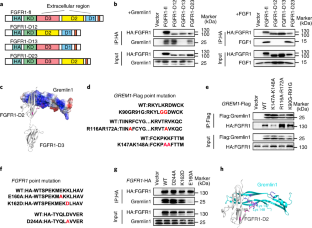

作者还发现Gremlin1的异常表达可以影响肿瘤细胞的可塑性,从而使得肿瘤细胞能够更好地应对环境改变(比如雄激素水平降低)对它们所造成的威胁。机制方面,本文首次证实,Gremlin1蛋白可以激活FGFR1,进而磷酸化ERK/MEK信号转导途径。应用FGFR1或者MAPK信号通路的拮抗剂则能够拮抗Gremlin1对前列腺癌的促进作用,而BMP配体或是BMP受体拮抗剂则不能干扰该蛋白对肿瘤细胞的影响。这些数据让作者猜测Gremlin1可以与FGFR1直接结合,是之前没有被发现的FGFR1新型配体。为此,作者利用计算机模拟软件预测了Gremlin1与FGFR1可能的结合构象,并基于此推测出两者结合的关键氨基酸位点,通过截断体、点突变等方式进一步证明Gremlin1与FGFR1之间存在配体-受体的直接结合,并且它们的结合方式与FGFR1经典受体FGF1不同。
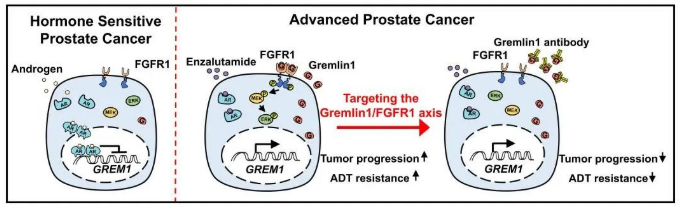
分泌蛋白具有容易靶向的特点,是目前新型治疗方案以及靶向药物开发的重要来源。在本研究中,作者使用苏州创胜医药集团有限公司开发的Gremlin1特异性抗体和前列腺自发瘤转基因小鼠模型以及人源性肿瘤组织移植模型,在体内验证Gremlin1特异性抗体对前列腺癌的治疗作用。实验发现,Gremlin1可以有效缓解前列腺癌进展,并在与临床抗雄药物恩杂鲁胺联合应用时有更加显著的治疗效果。这项研究发现了Gremlin1对前列腺癌肿瘤细胞可塑性和去势抵抗形成的重要作用,深入解析AR如何调控Gremlin1转录表达。作者创新性地发现Gremlin1可以与FGFR1结合,作为FGFR1的新型配体激活FGFR1/MAPK信号通路。同时本文为靶向治疗去势抵抗性前列腺癌提供了新型候选药物,具有重要的临床转化意义。
该工作主要由仁济医院临床干细胞中心、癌基因及相关基因国家重点实验室、上海市肿瘤研究所朱鹤研究员和高维强教授及苏州创胜医药集团有限公司的团队,并在仁济医院泌尿科主任薛蔚教授的大力支持下,共同完成。本文通讯作者朱鹤研究员和高维强教授,第一作者为程姹萍在站博士后和王金名在读博士。
文章链接:
Cheng, C., Wang, J., Xu, P. et al. Gremlin1 is a therapeutically targetable FGFR1 ligand that regulates lineage plasticity and castration resistance in prostate cancer. Nat Cancer 3, 565–580 (2022). https://doi.org/10.1038/s43018-022-00380-3
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#Nat#
47
#REM#
48
#抗性#
55
#新靶点#
40
#去势抵抗性前列腺癌#
55
#仁济医院#
44
#治疗新靶点#
37