Cell Prolif :重大进展 ,同济大学左为团队研究揭示新冠重症患者肺部干细胞可参与肺损伤修复
2020-10-29 椰子 iNature
新型冠状病毒感染导致的肺脏组织结构破坏,往往进展为严重的呼吸窘迫综合征 ( ARDS)并最终导致呼吸衰竭, 此为各类病毒性重症肺炎患者死亡的最根本原因。
目前新冠肺炎(COVID-19)疫情在全球范围内仍处于蔓延态势。根据世卫组织10月23日发布的统计数据,全球累计新冠肺炎确诊病例达到41570883例,累计死亡病例为1134940例。全球单日新增确诊病例445419例,为疫情暴发以来的新高。
2020年10月23日,同济大学医学院左为教授团队在Cell Proliferation 在线发表题为“Single-cell analysisidentified lung progenitor cells in COVID-19 patients”的研究论文,该研究揭示了新冠肺炎患者肺部的干细胞可能参与的再生修复机制。
新型冠状病毒感染导致的肺脏组织结构破坏,往往进展为严重的呼吸窘迫综合征 (Acute respiratory distress syndrome, ARDS)并最终导致呼吸衰竭, 此为各类病毒性重症肺炎患者死亡的最根本原因。已有的病理学等研究显示,ARDS的发病机制主要是冠状病毒攻击肺泡细胞之后诱发免疫反应,免疫细胞浸润导致肺泡血管内皮结构的破坏,使血浆、血浆蛋白和血细胞涌入肺间质和肺泡腔,形成肺水肿。由于肺泡上皮组织被破坏,水肿液大量涌入肺泡内,导致肺泡弥散功能受限,无法行使正常呼吸功能。同时,随着组织损伤的加剧,细胞进一步释放各类炎性因子形成所谓“细胞因子风暴(cytokine storm)”,最后彻底摧毁肺内大部分的肺泡和支气管呼吸结构,使得通气-血流比例严重失调,导致顽固的低氧血症以及最终患者的死亡。但是一些病人在肺部损伤后会完全恢复肺部功能,在新冠肺炎患者中肺部的再生修复机制和关键因素目前尚不明确。
左为教授团队在之前的研究中已经证实了人肺脏中存在着KRT5/P63双阳性细胞,这群细胞具有自我更新并分化成为不同类型成熟肺脏细胞的潜能。同时目前也有文献报道肺脏中的TM4SF1阳性的细胞,可以再生受损的支气管和肺泡组织。因此左为教授认为,在新冠肺炎患者肺部发生的肺部上皮组织再生过程中,研究肺干细胞在其中所发挥的再生修复的作用,如肺泡细胞的再生和上皮屏障的重新构建等。或许能揭示新冠肺炎病人肺部组织再生的机理。从而能够利用肺干细胞快速修复损伤的肺泡和支气管结构、进而重建稳定的气-血循环、改善血氧分压和氧饱和度,才能最大可能地挽救患者生命。这是从组织再生修复的病因学角度着手治疗病毒性肺炎的新思路。
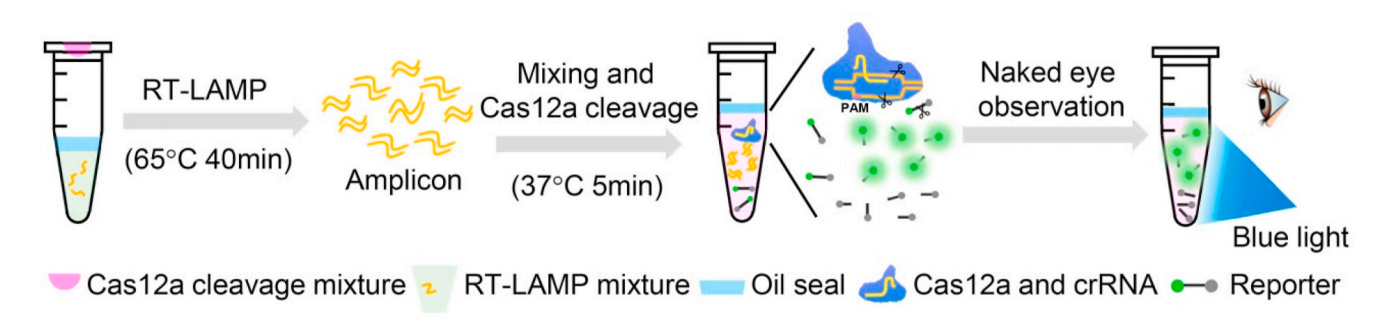
新冠疫情爆发后,左为团队即开始了针对新冠肺炎患者肺部的干细胞展开的研究。该项工作利用单细胞RNA测序分析技术,对新冠肺炎患者的支气管肺泡灌洗液(Bronchoalveolar lavage fluid,BALF)中的细胞组成情况进行了分析。收集BALF是一种很有效的取材方法,它可以提供整个下呼吸道的重要信息。左为团队对轻度症状和重度症状的新冠肺炎病人以及健康人的BALF进行了分析和比较。分析结果表明:相对于轻度症状的患者和健康人,在重度症状的新冠肺炎患者的BALF中,有显着增多的两群肺干细胞,分别为TM4SF1阳性和KRT5阳性。为了研究这两群肺干细胞在新冠肺炎患者体内所发挥的作用,左为团队的进一步研究表明:重度症状的新冠肺炎患者肺部的TM4SF1阳性的干细胞有更高的比例共表达成熟的肺泡细胞标志物,这揭示了TM4SF1阳性的干细胞在新冠肺炎患者的体内可能参与肺泡的再生和修复过程。
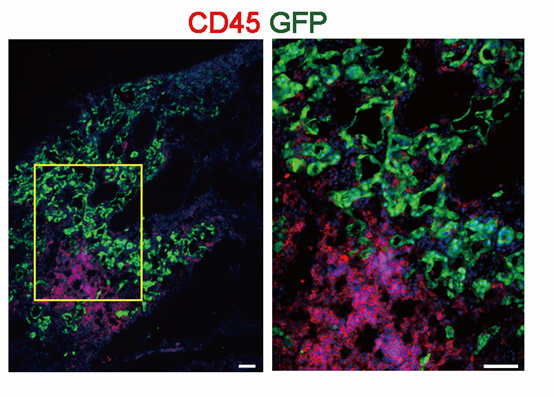
GFP阳性的肺干细胞(绿)阻止免疫细胞(红)的浸润
同时为了研究重度症状的新冠肺炎患者肺部增多的KRT5阳性干细胞的作用,左为团队把培养好的KRT5阳性的干细胞移植到了肺部损伤的小鼠肺脏。研究结果表明:移植的KRT5阳性的干细胞可以分化成肺泡屏障细胞(alveolar barrier cells,ABCs),修复破损的肺泡屏障细胞,从而避免破损的肺泡细胞受到免疫细胞的浸润。进一步研究表明:重度症状的新冠肺炎患者的BALF中有着更多的肺泡屏障细胞的再生。在对KRT5阳性干细胞的分子调控机制做了进一步研究后,左为团队发现KRT5阳性的干细胞在肺泡结构破损后受到了缺氧的刺激,从而调控其向肺泡屏障细胞的方向分化并修复再生破损的结构。
综上表明:在感染新冠肺炎后,重度症状的患者BALF中会显着增多两群肺干细胞,一种KRT5阳性的干细胞会分化成肺泡屏障细胞修复破损的结构,避免免疫细胞的浸润;同时,另一种TM4SF1阳性的干细胞会再生成有功能的肺泡细胞。两种肺干细胞在急性损伤下可以协同作用,完成肺泡组织结构的修复和再生。左为团队揭示了新冠肺炎患者肺部的干细胞可能参与的再生修复机制,对于后续利用干细胞治疗新冠肺炎患者,从组织再生修复的病因学角度着手治疗病毒性肺炎具有启发意义。当然,上述基于生物信息学分析的结果还有待于更多的后续深入研究论证。
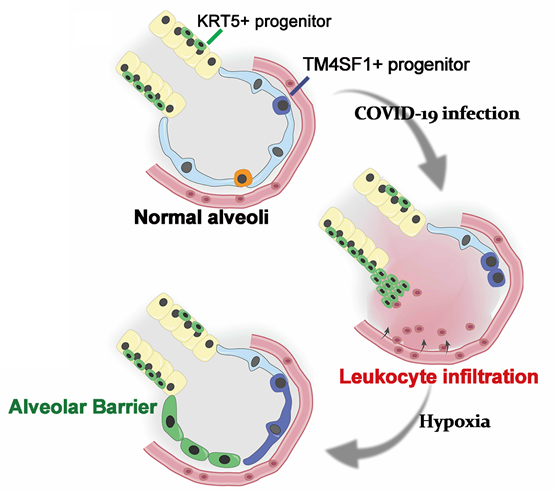
左为团队揭示的新冠病毒感染后干细胞参与的再生修复机制的示意图
左为教授为本论文的通讯作者。左为课题组博士生赵子贤、硕士生赵宇和博士生周悦青为本论文的共同第一作者。同济大学医学院、同济大学附属东方医院上海张江自主创新示范区干细胞转化医学基地干细胞制备与质检平台、苏州吉美瑞生医学科技有限公司等单位对研究提供了重要支持。论文致谢部分中,作者对在全球抗击疫情过程中牺牲的医务工作者致以了崇高敬意。
原始出处:
Zixian Zhao, Yu Zhao, Yueqing Zhou, et al.Single-cell analysis identified lung progenitor cells in COVID-19 patients.Cell Prolif. 2020 Oct 22;e12931. doi: 10.1111/cpr.12931.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#重大进展#
39
#Cell#
32
#CEL#
26
#同济大学#
44
#损伤修复#
41
#新冠重症患者#
35
干细胞是热点,但是进入临床仍然需要时间和临床疗效验证哦
55
#重症患者#
25
#损伤#
28
#肺损伤#
36