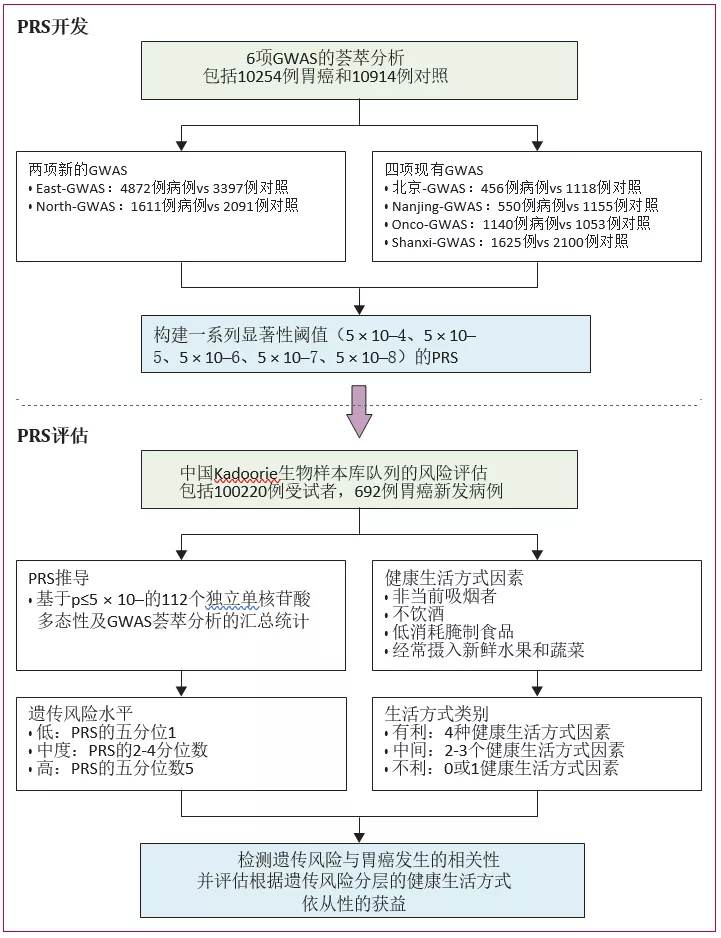
Nat Commun:Ⅱ期随机临床试验: 局部晚期胃癌患者新辅助FLOT与SOX疗法较量
2020-12-01 haibei MedSci原创
研究人员进行一项开放标签、双臂、II期随机干预临床试验(Dragon III;ClinicalTrials.gov:NCT03636893),以评估两种方案的安全性和有效性。
对于局部晚期胃癌(LAGC),在2006年MAGIC试验里程碑式的发表后,新辅助化疗出现了积极的趋势,该试验的结果最近甚至得到了亚洲国家临床试验结果的支持。
此外,最近的研究表明,新辅助化疗的耐受性良好,且不影响胃癌患者术后的发病率和死亡率。
德国一项大规模的研究明确显示,新辅助多西他赛、奥沙利铂、氟尿嘧啶和亮菌灵(FLOT方案)在病理反应和总生存期方面分别优于表柔比星、顺铂和氟尿嘧啶或卡培他滨(ECF或ECX方案)。以多西他赛为基础的三联化疗,即FLOT方案,在中国并不是一种常见的化疗方法,但有发表的研究表明,改良或标准FLOT方案在中国患者中是安全有效的。

多西他赛、奥沙利铂、氟尿嘧啶和亮丙瑞林的新辅助化疗(FLOT方案)在局部晚期可切除胃癌(LAGC)患者的病理反应和生存率方面表现出良好的效果。但在东方国家,替加福尔吉美拉西奥特拉西钾胶囊(S-1)加奥沙利铂(SOX方案)是首选的化疗方案。最近,研究人员进行一项开放标签、双臂、II期随机干预临床试验(Dragon III;ClinicalTrials.gov:NCT03636893),以评估两种方案的安全性和有效性。

LAGC患者被随机分配到胃切除术前接受4个周期的新辅助FLOT方案(40名患者)或3个周期的SOX方案(34名患者)。主要终点是比较原发肿瘤的完全(TRG1a)或次全(TRG1b)肿瘤转归分级。
两组不良反应或术后发病率和死亡率无显著差异。FLOT组与SOX组的肿瘤转归分级比例无显著差异。完全或次全TRG在FLOT组为20.0%,而SOX组为32.4%。
因此,该研究没有发现新辅助FLOT和SOX方案在本文报道的局部晚期胃癌的主要结果中存在统计学意义上的差异。
原始出处:
Birendra Kumar Sah et al. Neoadjuvant FLOT versus SOX phase II randomized clinical trial for patients with locally advanced gastric cancer. Nature Communications (2020).
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#局部晚期#
35
#Nat#
38
#FLOT#
41
#随机临床试验#
56
#新辅助#
36
#胃癌患者#
42
#COMMUN#
48
#晚期胃癌#
34
#局部#
31
#Nat Commun#也发表临床研究的文章?
79