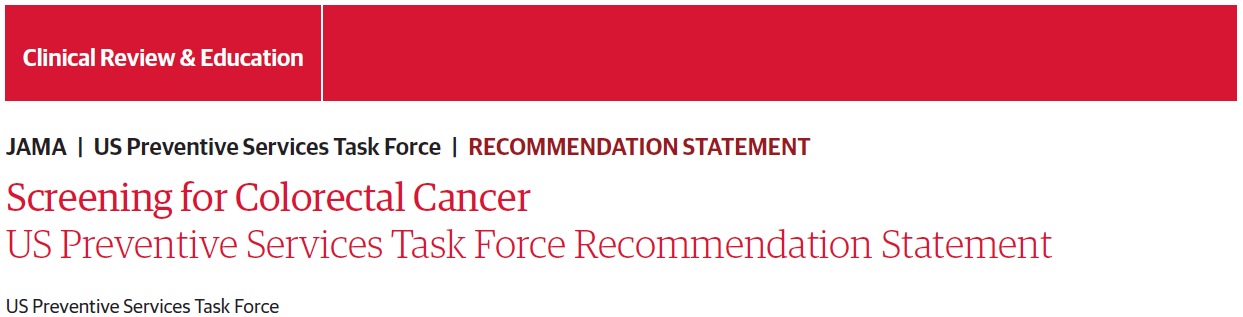
JAMA:USPSTF结直肠癌筛查最终建议:起始年龄从50岁更新为45岁
2021-05-19 Dr.Sun Nutrition & Health MedSci原创
美国预防医学工作组(USPSTF)的最终建议指出,结直肠癌筛查现在应从45岁开始,而不是50岁开始。
美国预防医学工作组(USPSTF)的最终建议指出,结直肠癌筛查现在应从45岁开始,而不是50岁开始。
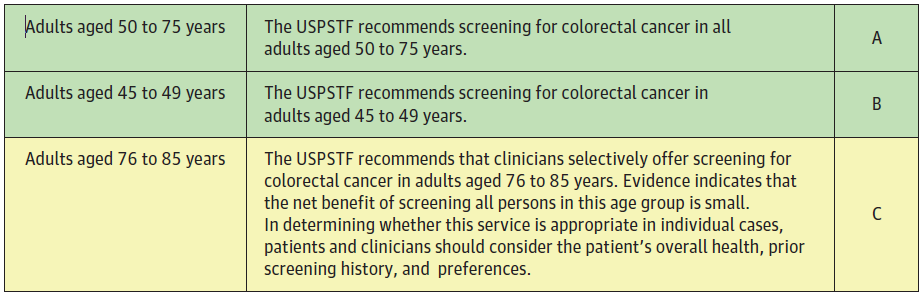
美国预防医学工作组(USPSTF)结直肠癌筛查建议摘要
该建议最后敲定了2020年10月发布的指南草案,并规定保险范围,以确保无论患者的保险状况如何,都能平等地获得CRC筛查。
USPSTF的最终建议也与美国癌症协会的建议一致,该协会在2018年将CRC筛查的开始年龄降低到45岁。
新指南JAMA社论的主要作者,马萨诸塞州波士顿丹娜—法伯癌症研究所年轻型结直肠癌中心主任Kimmie Ng评论道:“新的统计数据预测,到2040年,年轻型结直肠癌的发病率将惊人地上升,预计将成为20至49岁患者癌症死亡的主要原因。”
她强调:“我们必须采取大胆的步骤,将降低筛查开始年龄转化为CRC发病率和死亡率的显著下降。”
5月18日,美国预防医学工作组(USPSTF)建议和大量证据在JAMA在线发表。
CRC的风险因素
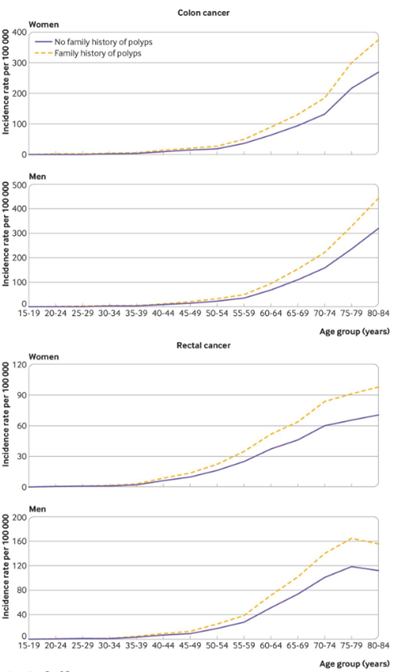
正如USPSTF作者指出的,年龄是CRC最重要的风险因素之一,近94%的CRC新发病例发生在45岁及以上的成年人中。CRC筛查开始年龄降低的证据基于模拟模型,表明45岁开始筛查与50岁开始筛查相比,预计与额外增加22至27生命年有关。
USPSTF继续建议对所有50至75岁的成年人进行CRC筛查,将筛查年龄降低到45岁确认了以下事实:在2020年,11%的结肠癌和15%的直肠癌发生在50岁以下的患者中。
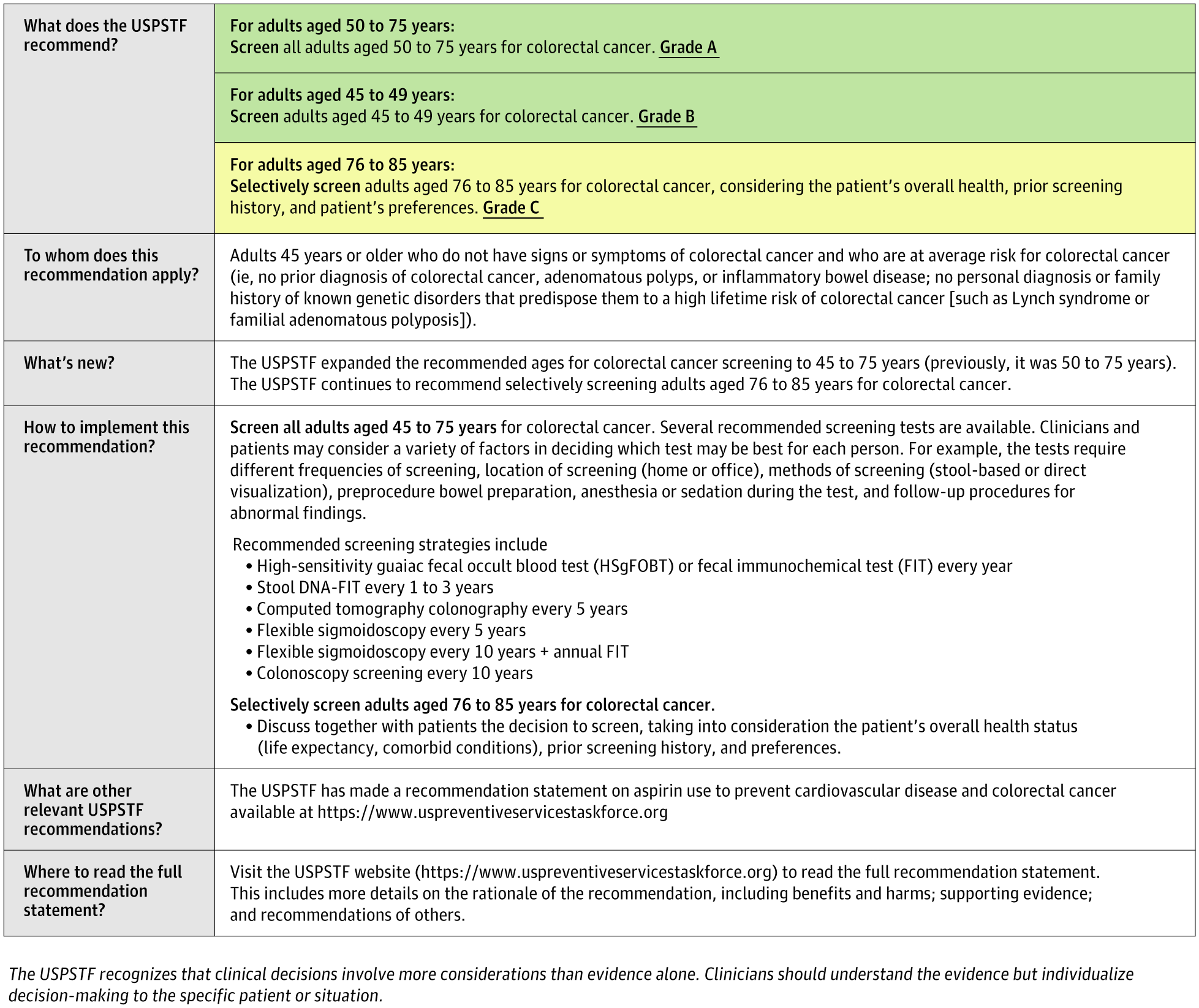
临床医生结直肠癌筛查摘要
USPSTF还继续得出结论,在以前接受过筛查的76至85岁成年人中,对CRC筛查有“低净获益”。
但是,筛查这一年龄组患者的决定应基于CRC的个体风险因素、患者的整体健康状况和个人偏好。也许不言而喻,这个年龄段从未接受过CRC筛查的成年人比之前接受过CRC筛查的成年人更有可能从CRC筛查中受益。
与先前2016年发布的指南类似,更新后的USPSTF建议继续提供筛查策略菜单,尽管每个筛查策略的筛查频率各不相同。推荐的筛查策略包括:
·高灵敏度愈创木脂粪便隐血检测或粪便免疫化学检测(FIT) 每年一次
·粪便DNA-FIT检测 每1到3年一次
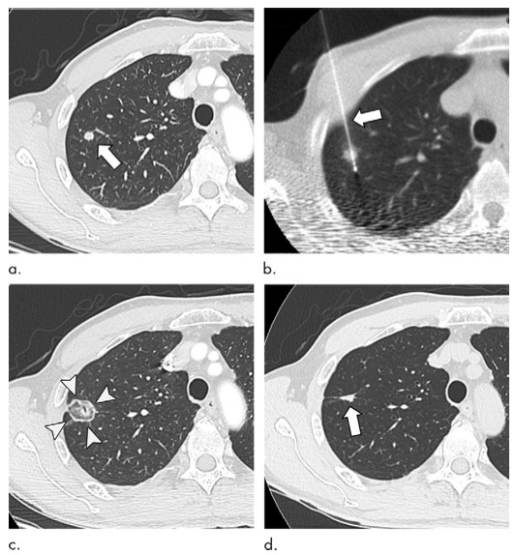
·CT结肠成像检查 每5年一次
·软式乙状结肠镜检查 每5年一次
·软式乙状结肠镜检查 每10年一次 加上FIT每年一次
·结肠镜筛查 每10年一次
USPSTF成员Martha Kubik在一份声明中说:“根据证据,有许多检查可以有效地筛查结直肠癌,正确的检查就是完成检查。”
符合条件的患者
Ng在社论中指出,目前,美国只有不到70%符合条件的患者接受了CRC筛查。此外,CRC对非裔美国人患者的影响不成比例,与其他患者群体相比,非裔美国人患CRC的可能性要高20%,死于CRC的可能性要高40%。与USPSTF建议一起发表的模型研究表明,无论种族和性别如何,筛查都具有同等的益处,这强调了筛查依从性的重要性,特别是在受CRC影响不成比例的患者群体中。
结直肠癌是男性和女性癌症死亡的第三大原因,预计2021年美国有52980人死于结直肠癌。结直肠癌在65至74岁的人群中最为常见。据估计,10.5%的新发结直肠癌病例发生在50岁以下的人。从2000-2002年至2014-2016年,40至49岁成年人的结直肠癌(特别是腺癌)发病率增加了近15%。2016年,美国符合条件的成年人有26%从未接受过结直肠癌筛查,2018年,31%的成年人迄今未接受过筛查。
原始出处:
US Preventive Services Task Force; Karina W Davidson, Michael J Barry et al. Screening for Colorectal Cancer: US Preventive Services Task Force Recommendation Statement. JAMA. 2021 May 18;325(19):1965-1977. doi: 10.1001/jama.2021.6238.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#45岁#
34
很好
63
#结直肠#
43
#USPSTF#
34
顶刊就是顶刊,谢谢梅斯带来这么高水平的研究报道,我们科里同事经常看梅斯,分享梅斯上的信息
0
疾病年龄日渐缩小
65