Nat Commun:NPM1突变的急性髓细胞性白血病独特亚型的生物学和治疗意义
2021-02-26 xiaozeng MedSci原创
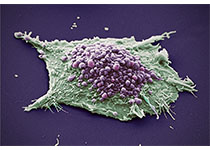
急性髓细胞性白血病(AML)作为一种遗传和生物学异质性疾病,其特征是突变型造血干细胞和祖细胞的克隆扩增和分化受损。
急性髓细胞性白血病(AML)作为一种遗传和生物学异质性疾病,其特征是突变型造血干细胞和祖细胞的克隆扩增和分化受损。患者之间的分子异质性对于AML的预后和治疗构成了重大挑战。
在修订的世界卫生组织(WHO)髓性白血病分类中,NPM1突变是其中一种独特的白血病遗传实体,且在患者的预后和治疗决策中起着至关重要的作用。
NPM1突变通常与诱导和巩固化疗后对患者生存的有利影响相关。然而,NPM1突变AML的大多数研究都集中在其他突变的同现上,而NPM1突变患者在基因表达水平上的异质性及其生物学意义目前尚未得到全面的研究。
NPM1突变AML患者可分为两种不同的分子亚型
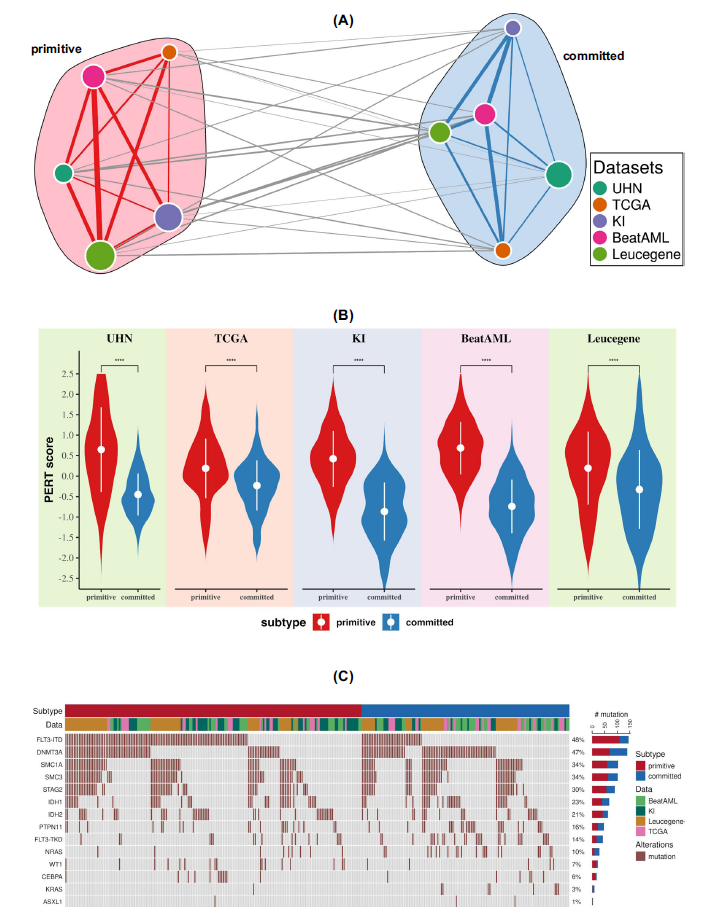
在该研究中,研究人员报告了携带NPM1突变AML患者中的两个不同亚型,根据干细胞标记的存在与否将其标记为原始型(primitive)和定型(committed)。使用基因表达(RNA-seq)、表观基因组(ATAC-seq)和免疫表型(CyToF)分析,研究人员将每种亚型与特定的分子特征、疾病分化状态和患者存活率相关联。
离体药物敏感性分析显示,不同亚型对于特定的激酶抑制剂具有不同的药物反应,而与FLT3-ITD的状态无关。进一步的研究也在独立的AML队列中验证了原始型和定型亚型的药物反应差异。
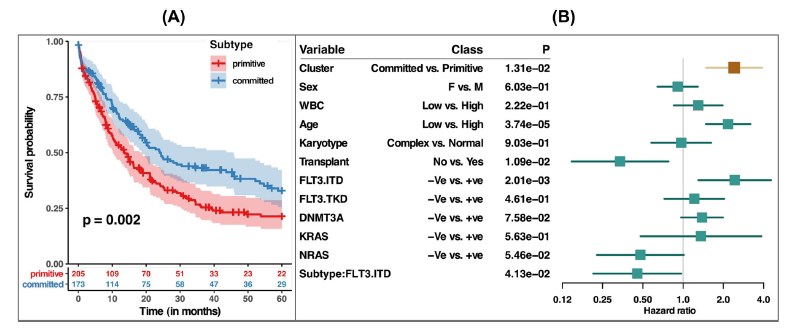
两种亚型与患者生存率相关
总而言之,该研究结果强调了基于干细胞特性的NPM1突变AML患者样本之间的异质性,并说明在原始型、FLT3-ITD缺失的病例中添加激酶抑制剂或具有治疗效益。
原始出处:
Mer, A.S., Heath, E.M., Madani Tonekaboni, S.A. et al. Biological and therapeutic implications of a unique subtype of NPM1 mutated AML. Nat Commun 12, 1054 (16 February 2021).
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#细胞性#
38
#COMMUN#
24
#PM1#
42
#治疗意义#
37
#Nat#
25
#髓细胞#
39
#急性髓细胞性白血病#
40
#NPM1#
49
#生物学#
31