JAMA Netw Open: HIV患者血CD4+ T细胞计数和病毒载量是否与认知障碍风险相关?
2021-01-18 MedSci原创 MedSci原创
了解可能导致HIV阳性个体神经精神和认知结果的神经生物学变化,对于识别有神经症状风险的个体、推动可能保护中枢神经系统的新疗法以及监测治疗反应至关重要。
尽管抗逆转录病毒联合疗法(cART)得到了更广泛的应用,但HIV-1感染仍然是一个全球公共卫生挑战。即使是接受治疗的慢性艾滋病毒感染患者,神经认知障碍也常常持续存在,影响生活质量。HIV阳性人群中神经认知障碍的患病率在不同的研究中有所不同:在一项综述中,有研究表明,近一半的HIV阳性个体存在认知障碍,但也有其他研究表明,受影响的人不到20%。这种变异性可能反映了病毒-宿主动力学和cART治疗状态的异质性。其他因素可能包括临床环境和地理区域的文化、社会经济和教育差异以及神经心理学测试方法,包括使用适当的规范性数据,以及处理神经和精神混杂因素。另一项使用标准神经心理学评估和适当规范性数据的研究回顾发现,即使是轻微的神经认知损伤,也与执行日常生活工具性活动的能力受到干扰之间存在着密切的联系。
识别与体内感染相关的神经解剖学途径可以描述这些缺陷背后的神经病理过程。然而,发表的来自相对较小的异质队列的神经影像学结果是不一致的,限制了迄今得出的结论的普遍性。有研究团队探索了大脑结构与最常用的HIV负担临床评估(CD4+ t细胞计数和病毒载量)的关系,研究结果发表在了JAMA Netw Open杂志上。
这项横断面研究建立了加强神经成像遗传学的HIV工作组,通过Meta分析(ENIGMA)联盟来汇集和协调来自现有HIV神经成像研究的数据。总的来说,来自非洲、亚洲、澳大利亚、欧洲和北美13项研究的1295名hiv阳性成年人的数据。在2014年11月1日至2019年12月31日的滚动基础上,从数据集中提取区域和全脑分割。
研究人员从T1加权磁共振图像中提取了8个大脑皮层下区域的体积估计数,以确定HIV阳性参与者当前免疫抑制的血浆标记物(CD4+ T细胞计数)或可检测的血浆病毒载量(dVL)的相关性。
经过质量评估后收集到1203名HIV阳性个体的数据。结果显示,较低的CD4+ T细胞计数与较小的海马和丘脑体积和较大的脑室有关;然而,在未进行cART治疗的参与者中,较低的CD4+ T细胞计数与较小的壳核体积相关。dVL与海马体积较小相关(d = 0.17;P = .005);在经cART治疗的参与者中,dVL也与较小的杏仁核体积相关(d = 0.23;P = 04)。
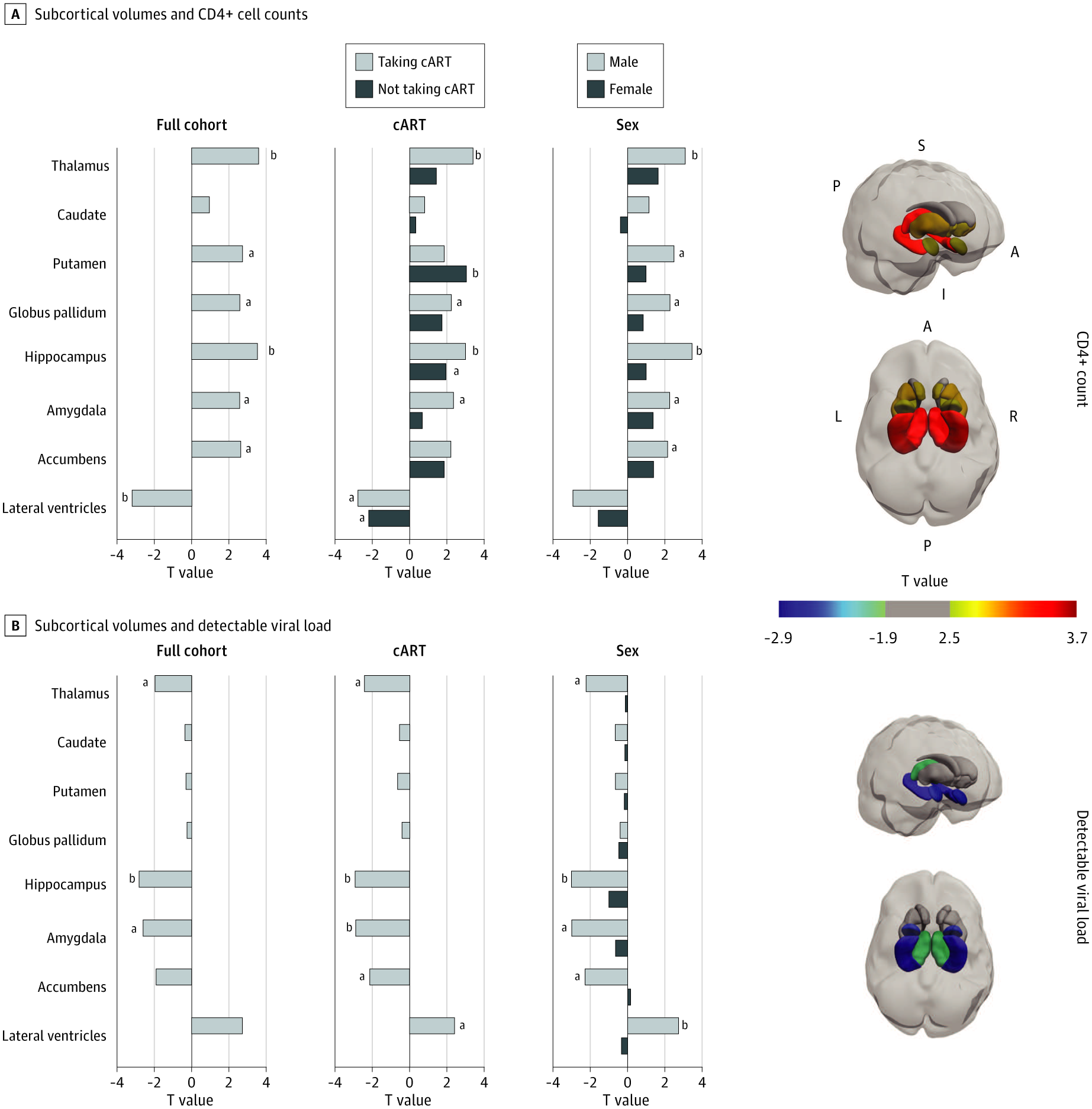
扫描时皮质下容积与CD4+ T细胞计数和可检测病毒载量之间的关系
总之,这项分析证明了一项全球合作倡议的可行性和实用性,可以了解艾滋病毒感染的神经特征。通过更大的合作努力,研究者将能够在有力的分析中评估可能调节神经系统结果的因素,包括cART治疗方案、共病、共感染、药物使用、社会经济因素和人口统计学因素,以及这种大脑结构差异的功能影响。了解可能导致HIV阳性个体神经精神和认知结果的神经生物学变化,对于识别有神经症状风险的个体、推动可能保护中枢神经系统的新疗法以及监测治疗反应至关重要。
参考文献:Nir TM, Fouche J, Ananworanich J, et al. Association of Immunosuppression and Viral Load With Subcortical Brain Volume in an International Sample of People Living With HIV. JAMA Netw Open. 2021;4(1):e2031190. doi:10.1001/jamanetworkopen.2020.31190
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#NET#
48
#HIV患者#
38
#CD4#
49
#PE#
46
#CD4+#
42
#病毒载量#
42
顶刊就是顶刊,谢谢梅斯带来这么高水平的研究报道,我们科里同事经常看梅斯,分享梅斯上的信息
67