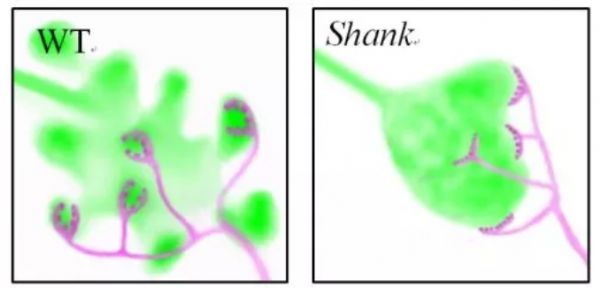
J NeuroSci:自闭症神经环路新机制
2017-11-08 佚名 大话精神
自闭症(autism spectrum disorder, ASD),是一类常见的神经发育疾病,发病率占普通人群的1%。ASD临床表现为人际交往障碍、行为方式刻板重复及兴趣狭窄。随着社会经济的发展和饮食生活习惯的改变,ASD的发病率有逐年上升的趋势,给社会和家庭带来巨大的经济和精神负担,已成为需要迫切关注的公共健康问题。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#ROS#
28
#神经环路#
25
#自闭#
26
谢谢分享!
82