Lancet Neurology:八种院前卒中量表检测疑似卒中患者颅内大血管闭塞的比较:一项前瞻性观察研究
2021-03-13 网络 网络
在全世界范围内,卒中是导致死亡或残疾的主要原因之一,尤其是在因近端颅内大血管闭塞而引起的缺血性脑卒中患者中。静脉溶栓和血管内血栓清除术已被证明对缺血性脑卒中患者有效,但其效果具有高度的时间依赖性。
在全世界范围内,卒中是导致死亡或残疾的主要原因之一,尤其是在因近端颅内大血管闭塞而引起的缺血性脑卒中患者中。静脉溶栓和血管内血栓清除术已被证明对缺血性脑卒中患者有效,但其效果具有高度的时间依赖性。由于血管内治疗的时效性,在院前快速确定疑似卒中患者的大血管闭塞对于优化预后至关重要。而院间转移是血管内治疗延迟的重要原因。院前卒中量表被建议用于选择性大血管闭塞的患者,以便将其直接转移到血管内介入中心。本研究的目的旨在前瞻性地验证八个院前卒中量表。
本文是一项多中心、前瞻性、观察性队列研究,研究对象是疑似中风的成年人(年龄≥18岁),他们被救护车送往荷兰西南部八家医院之一。疑似中风是通过阳性面部-手臂-言语-时间(FAST)测试来定义的。本研究纳入血糖至少为2.5 mmol/L的患者。中风症状出现后超过6小时的人被排除在分析之外。
经过训练后,医护人员使用移动应用程序对8个院前中风量表进行评估,分别是:快速动脉闭塞评估(RACE)、洛杉矶运动量表(LAMS)、辛辛那提中风分类评估工具(C-STAT)、凝视-面部手臂语言时间(G-FAST)、院前急性中风严重程度(PASS),辛辛那提院前卒中量表(CPSS)、方便掌握的现场评卒中分类(CG-FAST)和FAST-PLUS(面部-手臂-语言-时间+严重手臂或腿部运动缺陷)测试。主要结果是CT血管造影对缺血性中风伴近端颅内前循环大血管闭塞(aLVO)的临床诊断。院前卒中量表以受试者操作特征曲线(AUC)下的面积为表现,并与由急诊科临床医生评估的美国国立卫生研究院卒中量表(NIHSS)评分进行比较。
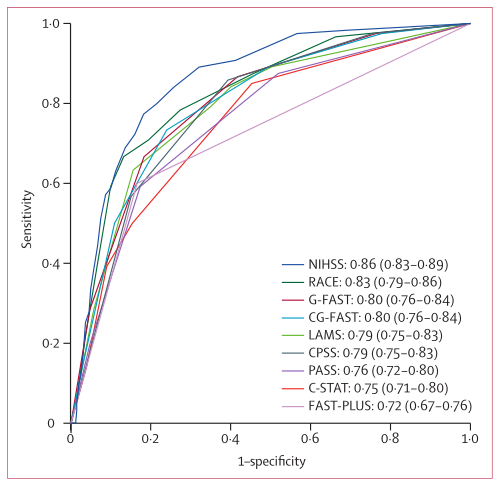
在2018年8月13日至2019年9月2日期间,医护人员确认了1039名疑似中风患者(中位年龄72岁[IQR 61-81]),其中120人(12%)被诊断为aLVO。在所有院前卒中量表中,RACE的AUC最高(0.83, 95%CI 0.79-0.86),其次是G-FAST(0.80, 0.76-0.84)、CG-FAST(0.80, 0.76-0.84)、LAMS(0.79, 0.75-0.83)、CPSS(0.79, 0.75-0.83)、PASS(0.76, 0.72-0.80)、C-STAT(0.75, 0.71-0.80)和FAST-PLUS(0.72, 0.67-0.76)。
综上所述,本文的研究发现,现场评估的RACE评分为5分或更高相当于40%或更高的aLVO风险(阳性预测值0.40),支持在大多数城市和郊区的临床实践中实施RACE(或具有类似阈值的其他院前卒中量表)。
各种量表在线使用:
洛杉矶院前卒中筛查(LAPSS)
急诊卒中识别评分量表(ROSIER)
神经科高危人群30天内再住院风险评估(Neuro R2评分)
缺血性卒中患者早期预后评估(S-SMART评分)
Duvekot, Martijne H CDippel, Diederik W.J. et al. Comparison of eight prehospital stroke scales to detect intracranial large-vessel occlusion in suspected stroke (PRESTO): a prospective observational study. The Lancet Neurology, Volume 20, Issue 3, 213 - 221
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#Lancet#
24
#观察研究#
29
#卒中患者#
25
#院前#
28
#大血管#
32
#前瞻性#
27
#Neurol#
30
#血管闭塞#
32
卒中虽然是临床上常见病,溶栓,取栓等血管内治疗也很成熟,但是仍然有很多未知问题有待认知!
39
顶刊就是不一样,质量很高,内容精彩!学到很多
52