JNER:基于外骨骼的物理治疗方案对亚急性中风康复期间非卧床患者的疗效:一项随机对照试验
2021-10-15 MedSci原创 MedSci原创
在亚急性中风康复期间,需要物理治疗帮助患者康复。电动外骨骼已经被开发出来,可以帮助下肢无力的人进行重复的地面步态训练。本研究的目的是确定非卧床中风患者亚急性康复期间基于外骨骼的物理治疗训练的疗效。
在亚急性中风康复期间,需要物理治疗帮助患者康复。电动外骨骼已经被开发出来,可以帮助下肢无力的人进行重复的地面步态训练。本研究的主要目的是评估基于外骨骼的物理治疗方案对亚急性中风康复期间步行能力恢复的影响。与接受标准物理治疗的患者相比,在物理治疗期间定期使用外骨骼的非卧床患者在出院时具有更大的行走独立性。第二个目标是评估基于外骨骼的物理治疗在出院时和6个月后对额外步行和活动结果(如速度)、腿部运动障碍、平衡、认知、卒中后抑郁和生活质量的影响。本文发表在《Journal of NeuroEngineering and Rehabilitation》。
在3家住院康复医院进行了一项员盲法随机对照试验。亚急性脑卒中患者(< 3个月)的患者在没有实质性协助的情况下无法行走(功能性步行分类评分为0或1),被随机分配在康复期间接受外骨骼或标准物理治疗,直到出院或最多8周。实验方案将75%的标准物理治疗课程替换为基于外骨骼的个性化课程,以增加站立和行走的重复性。主要结果是步行能力测量,使用功能性步行分类进行测量。次要结果是步态速度、6分钟步行测试的步行距离、实现独立步态的天数、下肢运动功能(Fugl-Meyer评估)、Berg平衡量表、患者健康问卷、蒙特利尔认知评估和36项简式调查,在干预后和6个月后测得。
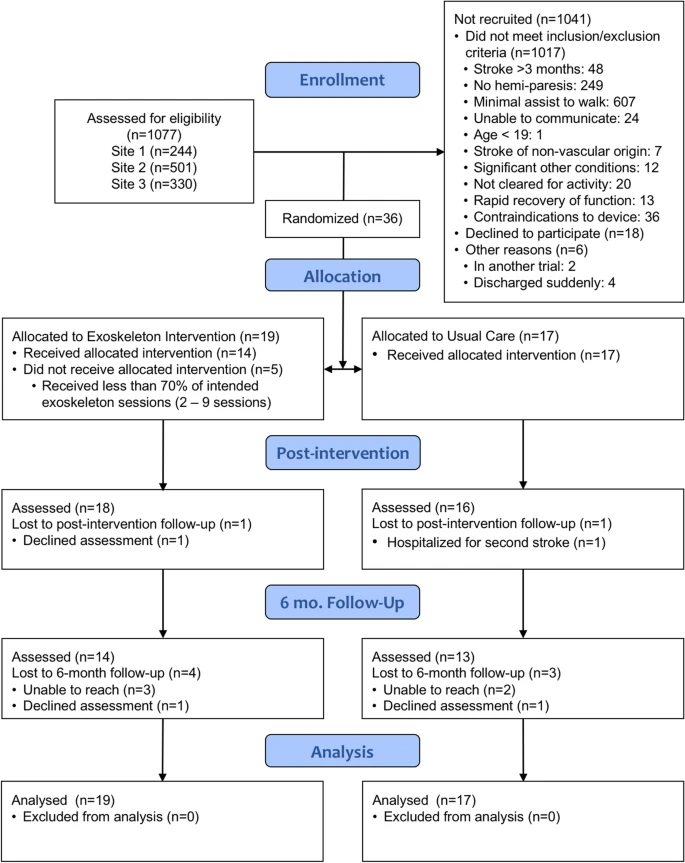
研究流程
36名中风患者(中风后平均39天)被随机分组(外骨骼=19,常规护理=17)。在意向治疗分析中,在干预后或6个月后,在主要或次要结果方面未发现组间差异。随机分为外骨骼组的五名参与者没有按计划接受方案。治疗后分析发现,坚持外骨骼物理疗法的患者更早地恢复了独立行走(p = 0.03),步速加快(p = 0.04)和6MWT(p = 6个月时为0.03);然而,在按方案分析中,这些差异并不显著。未报告严重不良事件。
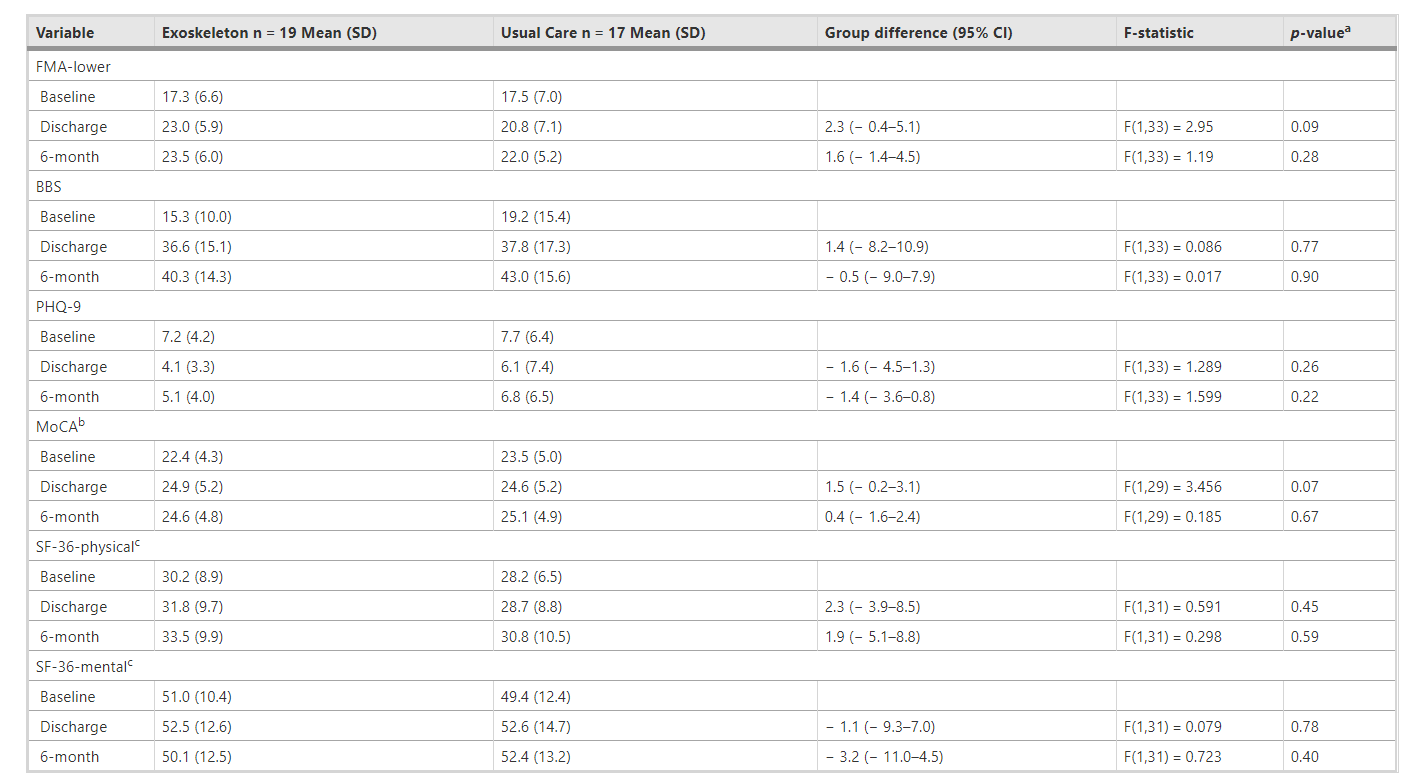
损害、平衡、情绪、认知和生活质量的次要结果
研究的参与者可能没有达到足够的训练阈值,未在步行恢复中产生巨大的收益,部分原因是基于外骨骼的步态干预的灵活性和可变性。研究参与者每周参加2.9次外骨骼训练,以代替他们的标准物理治疗(约占每周治疗的75%),患者可能没有达到与先前机电设备外骨骼研究中提供的相同的日常步行练习(即每周5天或作为附加治疗)强度。与标准物理治疗没有显著差异并不意味着机器人外骨骼不应用于临床实践。事实上,治疗前和方案分析表明,在运动功能和行走的物理治疗过程中使用外骨骼具有潜在的好处。
这项研究发现,与标准护理相比,基于外骨骼的物理治疗不会导致行走独立性的更大改善,但可以安全地进行,而且不会损害患者的预后。
Louie, D.R., Mortenson, W.B., Durocher, M. et al. Efficacy of an exoskeleton-based physical therapy program for non-ambulatory patients during subacute stroke rehabilitation: a randomized controlled trial. J NeuroEngineering Rehabil 18, 149 (2021). https://doi.org/10.1186/s12984-021-00942-z
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言














#对照#
37
#治疗方案#
65
#外骨骼#
0
#康复期#
42
#对照试验#
43
#随机对照试验#
40