Liver Cancer:阿特珠单抗+贝伐单抗可显著延长中国晚期HCC患者的生存期!
2021-08-23 Nebula MedSci原创
与索拉非尼单药治疗相比,阿特珠单抗联合贝伐单抗也可显著延长中国晚期 HCC 患者的无进展生存期和总生存期
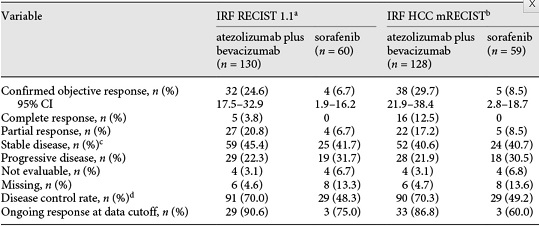
在IMbrave150试验中,与索拉非尼相比,阿特珠单抗联合贝伐单抗可显著延长不可切除的肝细胞癌(HCC)患者的无进展生存期(PFS)和总生存期(OS)。本文报告了对该试验中国患者亚组的疗效和安全性分析结果。
IMbrave150是一项全球性的、随机的、开放标签的3期试验,招募了未进行过系统治疗的不可切除的HCC患者。受试患者被随机(2:1)分至两组,分别接受静脉阿特珠单抗(1200 mg)联合贝伐单抗(15 mg/kg)(1次/3周)或索拉非尼(400 mg,2次/日)治疗,直到出现不可耐受的毒性或丧失临床意义。主要终点是OS和PFS。
2018年4月16日至2019年4月8日期间,共招募了194位中国患者(137位是在整体研究中,57位是在中国扩展研究阶段),其中133位接受了阿特珠单抗联合贝伐单抗治疗,61位接受的索拉非尼治疗。
两组的OS和PFS
截止2019年8月29日,联合组和索拉非尼组的中位OS分别是未达到 vs 11.4个月(校正风险比[HR] 0.44;95%CI 0.25-0.76);中位PFS分别是5.7 vs 3.2个月(HR 0.60;95%CI 0.40-0.90)。
不良反应事件
联合组和索拉非尼组3-4级不良反应事件(AE)的发生率分别是59.1%(78/132)和46.6%(27/58)。联合组最常见的3-4级AE为高血压(15.2%),其他高级别不良反应的发生率都不高。
综上,与索拉非尼单药治疗相比,阿特珠单抗联合贝伐单抗也可显著延长中国晚期 HCC 患者的 PFS 和 OS,提示该联合方案有可能成为中国不可切除 HCC 患者的一种有望改变临床实践的治疗方法。
原始出处:
Qin Shukui,Ren Zhenggang,Feng Yin-Hsun et al. Atezolizumab plus Bevacizumab versus Sorafenib in the Chinese Subpopulation with Unresectable Hepatocellular Carcinoma: Phase 3 Randomized, Open-Label IMbrave150 Study.[J] .Liver Cancer, 2021, 10: 296-308. https://doi.org/10.1159/000513486
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言














#贝伐单抗#
65
#晚期HCC#
29
#HCC#
40
#生存期#
35
#贝伐#
29
学习了,谢谢分享
78
期待更大人群的IV期研究
69
学习了,又多了种治疗方法
64
谢谢分享
60
学习了,谢谢分享
52