JAHA:心脏移植婴儿发生严重原发性移植物功能障碍的危险因素
2021-06-29 MedSci原创 MedSci原创
发生严重PGD的接受HT婴儿移植物存活率很低。尽管一些受者水平的危险因素是不可改变的,但避免可改变的危险因素可能会降低发生严重PGD的风险。
既往研究表明,接受心脏移植 (HT)的婴儿发生严重原发性移植物功能障碍 (PGD) 的风险高于年龄较大的儿童。

近日,心血管疾病领域权威杂志JAHA上发表了一篇研究文章,研究人员旨在明确接受HT婴儿发生严重PGD的危险因素。
 研究人员使用美国器官采购和移植网络数据库确定了1996年至2015年期间年龄1岁以内的所有接受HT的婴儿。研究人员将他们的数据与ELSO(体外生命支持组织)注册数据相关联,以识别那些患有严重PGD的婴儿,严重PGD定义是在HT后2天内开始对PGD进行体外膜氧合支持。研究人员使用多变量Logistic回归来评估发生严重PGD的风险因素。
研究人员使用美国器官采购和移植网络数据库确定了1996年至2015年期间年龄1岁以内的所有接受HT的婴儿。研究人员将他们的数据与ELSO(体外生命支持组织)注册数据相关联,以识别那些患有严重PGD的婴儿,严重PGD定义是在HT后2天内开始对PGD进行体外膜氧合支持。研究人员使用多变量Logistic回归来评估发生严重PGD的风险因素。
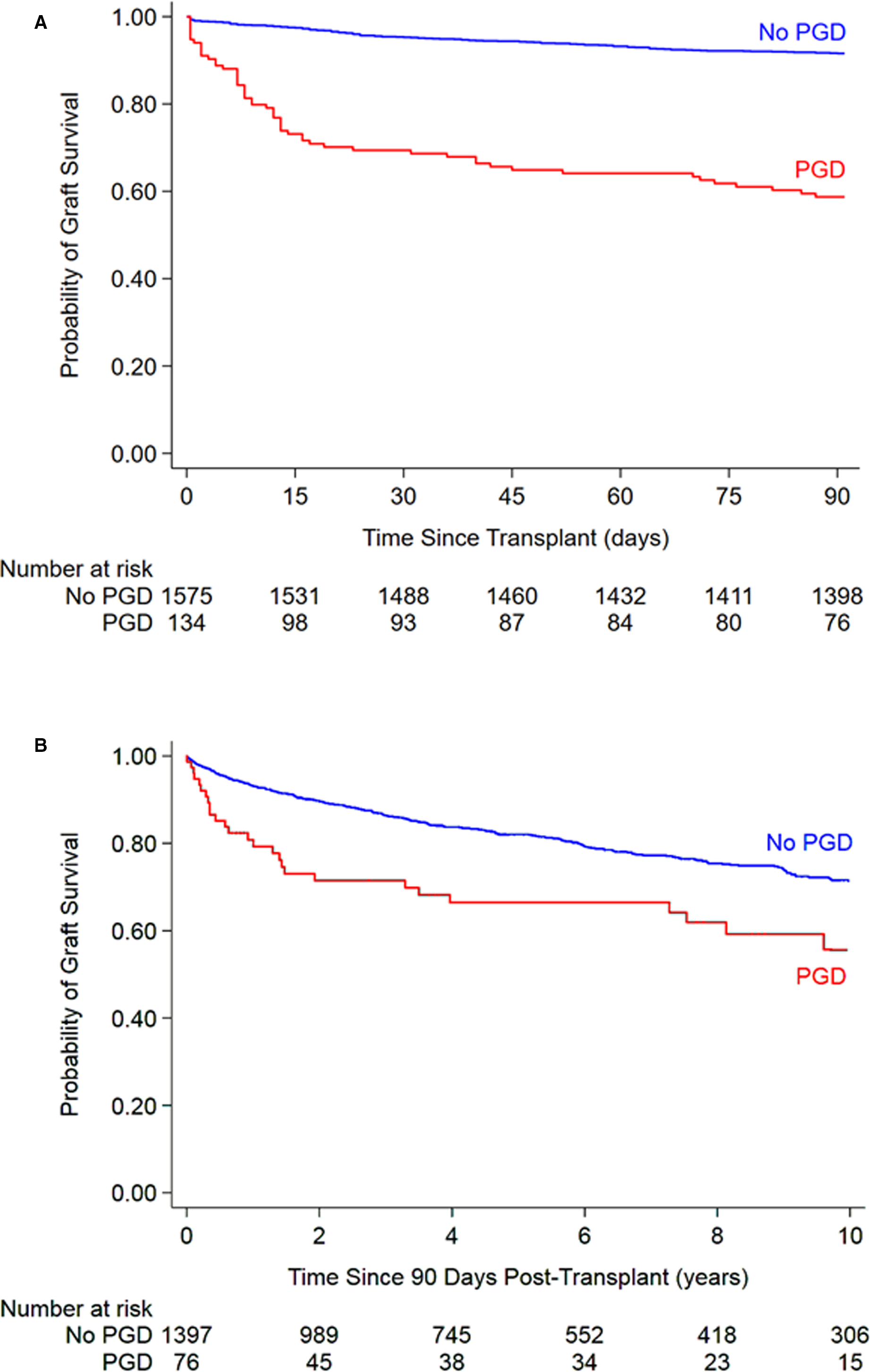 移植物生存率
移植物生存率
在参与分析的1718名婴儿中,600名(35%)婴儿小于90天,1079名(63%)患有先天性心脏病。总体而言,134名(7.8%)婴儿发展为严重PGD;95名(71%)婴儿在HT当天开始进行体外膜氧合支持,第二天有34名(25%)婴儿,第二天有5名(4%)婴儿。在校正分析中,接受HT的婴儿先天性心脏病、体外膜肺氧合或移植时双心室辅助装置支持、受者血型为AB型、供受者体重比<0.9和移植物缺血时间≥4小时与严重PGD的发生独立相关,而在HT时左心室辅助装置支持则不然。发生严重PGD的婴儿一年内移植物存活率为48%,而没有发生严重PGD的婴儿则为87%。
由此可见,发生严重PGD的接受HT婴儿移植物存活率很低。尽管一些受者水平的危险因素是不可改变的,但避免可改变的危险因素可能会降低发生严重PGD的风险。
原始出处:
Tajinder P. Singh.et al.Risk Factors for Severe Primary Graft Dysfunction in Infants Following Heart Transplant.J AM HEART ASSOC.2021.https://www.ahajournals.org/doi/10.1161/JAHA.121.021082
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#原发性#
33
#植物#
38
#AHA#
36
#功能障碍#
32
#移植物#
37