JNCI:三种PD-L1免疫组化分析方法对比及与三阴性乳腺癌患者治疗预后的相关性
2021-06-10 MedSci原创 MedSci原创
22C3和SP263检测相比SP142检出的PD-L1阳性率(IC≥1%)更高
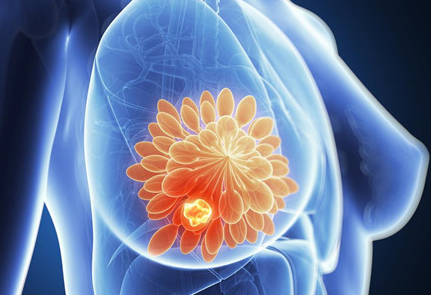
在3期IMpassion130研究中,阿特珠单抗联合nab-紫杉醇(A+nP)在PD-L1阳性(肿瘤浸润免疫细胞[IC]≥1%;SP142免疫组化[IHC])晚期/转移性三阴性乳腺癌(TNBC)患者中展现出了临床效益。
本研究旨在评估其他两种PD-L1检测方法是否与SP142和患者相关的临床预后一致。
采用IHC检测了614位患者(68.1%的患者为意向治疗人群)的样本中IC的PD-L1状态(VENTANA SP142、SP263、Dako 22C3)或作为联合阳性评分(CPS;22C3)。
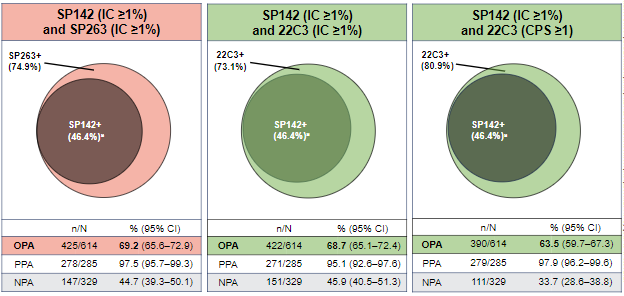
三种检测方法的阳性率
采用SP142、SP263和22C3实验,PD-L1 IC≥1%的概率分别为46.4%(95% CI 42.5–50.4%)、74.9%(71.5-78.3%)和73.1%(69/6-76.6%);80.9%的样本22C3实验的CPS≥1。在IC≥1% (+) 时,SP142 与SP263和22C3的分析一致性分别为 69.2% 和 68.7%。几乎所有 SP142+病例都被其他检测捕获到(双阳性),但是,部分SP263+(29.6%)和22C3+(29.0%)病例在SP142检测中为阴性(单阳性)。
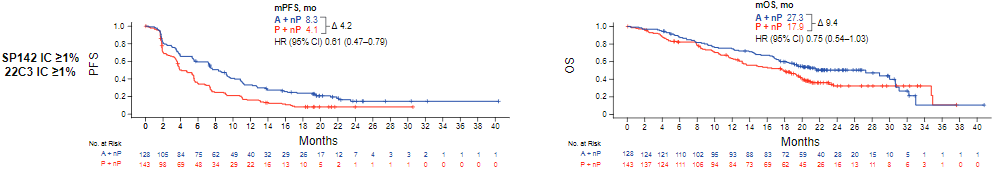
SP142+和22C3+患者采用A+nP vs P+nP治疗的PFS和OS
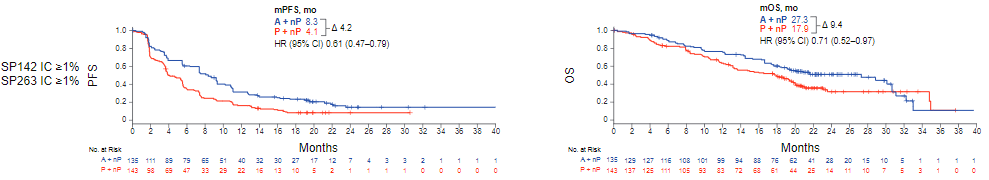
SP142+和SP263+患者采用A+nP vs P+nP治疗的PFS和OS
在SP263+和22C3+患者中,A+nP临床活性对比安慰剂+nP(PFS风险比[HR] 0.64-0.68;总存活率[OS]HR:0.75-0.79)是由双阳性(PFS HR 0.60–0.61; OS HR=0.71–0.75)而非单阳性(PFS HR=0.68–0.81; OS HR=0.87–0.95)驱动的。SP263(IC≥4%)和22C3(CPS≥10)与 SP142 IC≥1% 的协调临界值的一致性低于标准(约75%)。
总之,22C3和SP263检测相比SP142可鉴定出更多的PD-L1阳性(IC≥1%)的患者。未观察到不同检测方法间的分析等效性。在22C3和SP263 PD-L1阳性 (IC≥1%) 人群中,SP142 PD-L1 IC≥1%的患者从A+nP治疗中获得了持续改善的临床效益。
原始出处:
Rugo Hope S,Loi Sherene,Adams Sylvia et al. PD-L1 Immunohistochemistry Assay Comparison in Atezolizumab plus nab-Paclitaxel-Treated Advanced Triple-Negative Breast Cancer.[J] .J Natl Cancer Inst, 2021, https://doi.org/10.1093/jnci/djab108
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#阴性乳腺癌#
0
#相关性#
30
#NCI#
35
#PD-L1#
0
#免疫组化#
41
#三阴性#
0
#乳腺癌患者#
29